Chapter 10: Upper Extremity
Objectives:
- Describe the functional motions of the shoulder and the primary muscles causing abduction, adduction, flexion, extension, internal rotation and external rotation
- Describe the functional motions of the scapula and the primary muscles causing depression, elevation, upward rotation and downward rotation, protraction and retraction
- Identify the 17 muscles that attach to the scapula and associated actions
- Describe the functional motions of the elbow and the primary muscles causing flexion, extension, supination, pronation, adduction and abduction and their attachments and innervations
- Describe somatic dysfunctions of the elbow: anterior radial head, posterior radial head, adduction dysfunction, abduction dysfunction, and interosseous membrane restriction
- Describe motion of the radial head with regard to wrist abduction/adduction and the parallelogram effect and carrying angle
- Describe the motions of the wrist and the primary muscles that cause flexion, extension, adduction and abduction of the wrist and their attachments and innervations
- Describe the motions of the fingers and the primary muscles that cause flexion, extension, adduction and abduction of the fingers and their attachments and innervations
- Describe the motions of the thumb and the primary muscles that cause flexion, extension, adduction abduction, and opposition of the thumb and their attachments and innervations
- Recognize somatic dysfunctions of the carpal bones: anterior displacement and posterior displacement
- Describe the positions of the carpal bones in the hand as well as their relation to one another
- Identify the most commonly fractured carpal bones
- Describe the etiology of carpal tunnel syndrome and associated osteopathic treatments
Shoulder Anatomy
This section is an extension of Chapter 5, which dealt mainly with the clavicle and the sternum but dealt superficially with the shoulder and upper extremity. The upper extremity is made of three true joints: the glenohumeral joint, the acromioclavicular joint, and the sternoclavicular joint. The articulations of the upper extremity include the scapulothoracic articulation, the subacromial articulation, and the bicipital groove.
The glenohumeral joint contains the glenoid fossa surrounded by a ring of cartilage called a labrum, which deepens the pocket and allows for better conformity. The acromioclavicular joint connects the acromion (which is part of the scapula) and the clavicle. During structural examination of the shoulder: anteriorly, the sternoclavicular joint, the clavicles, the acromioclavicular joint, the coracoid process, the bicipital groove, and the spine of the scapula should be evaluated; posteriorly, the vertebral border of the scapula, the spine of the scapula (at the level of T3), the inferior angle of the scapula (at the level of T7), the medial border of the scapula, the lateral border of the scapula, and the acromion should be assessed. The shoulder is the site of multiple overlapping muscles and a distributor of tension.
There are 17 muscles which attach to the scapula:
- Serratus anterior+
- Trapezius+
- Teres major+
- Rhomboid major+
- Rhomboid minor+
- Latissimus dorsi+
- Deltoid+
- Levator scapulae+
- Pectoralis minor +
- Supraspintaus
- Infraspinatus
- Teres minor
- Subscapularis
- Coracobrachialis
- Omohyoid
- Biceps brachii
- Triceps brachii
+ These muscles have been discussed in Chapters 4 and 5 and will not be repeated here.
Table 10.1 details the primary muscles of the shoulder:
| Shoulder muscles | Flexors:
|
Extensors:
|
Adductors:
|
Abductors:
|
External rotators:
|
Internal rotators:
|
Scapular elevators:
|
Scapular protractor:
|
|---|
The muscles that comprise the rotator cuff of the shoulder include:
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Supraspinatus | Supraspinous fossa of the scapula | Greater tuberosity of the humerus | Abduction | Suprascapular nerve (C4-C6) | 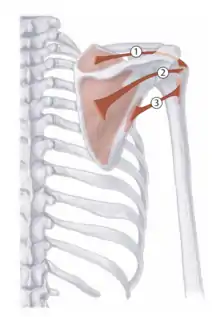 1 - Supraspinatus |
| Infraspinatus | Infraspinous fossa of the scapula | Greater tuberosity of the humerus | External rotation | Suprascapular nerve (C4-C6) | 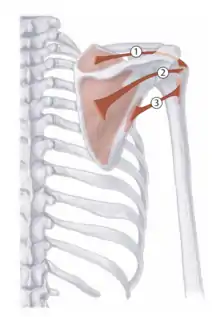 2 - Infraspinatus |
| Teres minor | Lateral border of the scapula | Greater tuberosity of the humerus | External rotation | Axillary nerve (C5-C6) | 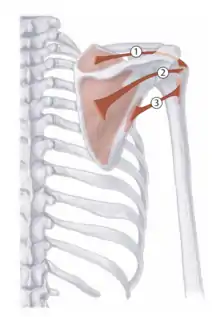 3 - Teres minor |
| Subscapularis | Subscapular fossa of the scapula | Lesser tuberosity of the humerus | Internal rotation | Subscapular nerve (C5-C6) |  4 - Subscapularis |
Table 10.2 - Muscles of the rotator cuff
Additional muscles that play an important role in the structure and function of the shoulder include:
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Pectoralis major |
|
Crest of the greater tuberosity of the humerus |
|
Medial and lateral pectoral nerves (C5-T1) | 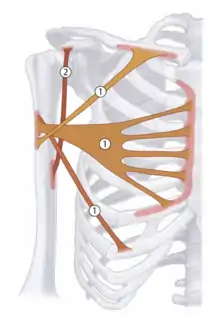 1 - Pectoralis Major |
| Coracobrachialis | Coracoid process of the scapula | Humerus | Adduction and internal rotation | Musculocutaneous nerve (C6-C7) | 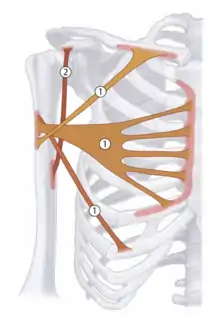 2 - Coracobrachialis |
| Omohyoid | Superior border of the scapula | Body of the hyoid bone |
|
Ansa cervicalis of the cevical plexus (C1-C4) | 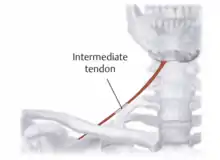 Omohyoid |
Table 10.3 - Additional muscles that attach to the scapula
The biceps brachii and triceps brachii will be covered in the section Anatomy of the Elbow.
Shoulder Somatic Dysfunctions
Shoulder somatic dysfunctions can be diagnosed using Spencer's technique (see Treatment of Shoulder Somatic Dysfunctions). Additionally, hypertonic supraspinatus, subscapularis, levator scapulae, and pectoralis minor muscles can decrease shoulder range of motion. Proximally, thoracic and clavicular somatic dysfunctions may effect on shoulder function. Distally, somatic dysfunctions on the elbow can also affect shoulder function.
Treatment of Shoulder Somatic Dysfunctions
Spencer's technique is used to evaluate the shoulder and can be used as both a diagnostic test and can be converted into a muscle energy or articulatory treatment. The goals of the Spencer technique are to improve shoulder mechanics and range of motion, stretch local tissues, improving lymphatic flow, and to improve circulatory flow.
The stages are:
| Flexion | Shoulder flexion with elbow extension |  1 - Shoulder Flexion |
|---|---|---|
| Extension | Shoulder extension with elbow flexion |  2 - Shoulder Extension |
| Circumduction with compression | Abduct to 90 degrees, stabilize the shoulder, flex the elbow to 90 degrees while compressing the elbow toward the shoulder joint and rotating clockwise and counterclockwise while increasing the range of motion in concentric circles |  3 - Shoulder Circumduction with Compression |
| Circumduction with traction | Abduct to 90 degrees, stabilize shoulder, extend the arm, compress and rotate either clockwise or counterclockwise while increasing the range of motion in concentric circles |  4 - Shoulder Circumduction with Traction |
| Internal rotation | Place the patient’s wrist and hand behind the back to abduct the shoulder to 45 degrees and gently pull the elbow forward |  5 - Shoulder Abduction External Rotation |
| Adduction/External rotation | This coupled motion is assessed by having the patient’s arm flexed such that the elbow is in front of the chest with the wrist resting on the physician’s forearm as the physician adducts the shoulder |  6 - Shoulder Internal Rotation |
| Abduction | With the leg straight, it is taken to its abduction barrier |  7 - Shoulder Abduction |
| Traction/Distraction in Abduction | Place the patient's hand on the physician’s shoulder and milk the deltoid muscle by interlocking the fingers distal to the acromion process |  8 - Shoulder Traction |
Spencer's technique can be converted into an articulatory technique or a post-isometric muscle energy technique if a barrier is appreciated. Following treatment, the dysfunction is reassessed in the same way that it was initially assessed. Be sure to correctly diagnose the somatic dysfunction and, if treating with a direct technique such as muscle energy, the appropriate restrictive barrier is engaged.
| Treating Spencer's technique somatic dysfunctions |
|
|---|
An additionally useful technique in the assessment and treatment of the shoulder is direct scapulothoracic articulation.
| Example: Scapulothoracic articulation of the right shoulder: |
|---|
| To perform scapulothoracic articulation of the right shoulder, the patient will lie in a left lateral recumbent position with the physician standing in front of the patient, facing the patient. The cephalad hand is placed over the right shoulder with the interspace of the thumb and index finger contacting the clavicle and the finger pads contacting the superior medial angle of the scapula. The caudad and is placed under the patient’s right arm along the inferior scapular border while a gentle compression is added. The range of motion is assessed in superior and inferior directions to determine ease/bind of the underlying myofascial elements. |
Counterstrain tenderpoints and treatments for selected upper extremity muscles:
| Tenderpoint+ | Location | Treatment position (initial setup) | Acronym | Figure (from Nicholas) |
|---|---|---|---|---|
| Supraspinatus | Mid-supraspinatus muscle just superior to the spine of the scapula | The patient lays supine. The tenderpoint is palpated and the arm is flexed, abducted, and externally rotated. | F Abd ER |  Supraspinatus CS |
| Levator scapulae | At the superior angle of the scapula | The patient lays prone, head rotated away from the side of the dysfunction, and the shoulder is internally rotated, abducted, and traction is applied. | IR Abd traction | 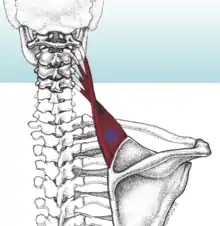 Levator Scapulae CS |
| Subscapularis | At the anterolateral border of the scapula on the subscapularis muscle | The patient lays supine, the shoulder is extended and internally rotated. | E IR | 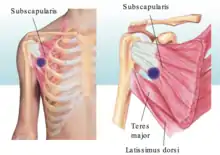 Subscapularis CS |
Elbow and Forearm Anatomy
The elbow is the truest hinge joint in the body. It is comprised of three bones and three articulations. The three bones that make up the elbow are the radius, the ulna, and the humerus. The humeroulnar joint is a direct articulation between the olecranon and the trochlea. Deviation determines the carrying angle. The humeroradial joint has articulation aided by ligaments. The radial head flexes against the capitulum. The proximal radioulnar joint allows for pronation and supination. The radial head can move clockwise or counterclockwise. The ulna deviates laterally with pronation.
There are four ligaments at the elbow: the ulnar collateral ligament, the radial collateral ligament, the radial collateral ligament, the annular ligament, and the anterior ligament. The ulnar collateral ligament is divided into anterior and posterior portions; it functions to protect against valgus strain. The radial collateral ligament is continuous with the annular ligament. It is divided into medial and lateral portions; it functions to protect from varus strain. The annular ligament completely surrounds the radial head, allows articulation of the humeroradial joint, and is the primary support for pronation and supination. The anterior ligament is divided into radial and ulnar portions and is a general stabilizer in all planes of motion.
The interosseous membrane is a major shock absorber. It bridges almost the entire gap from the proximal to distal radioulnar joints. (An analogous structure is present between the tibia and the fibula.)
Selected muscles involved in elbow motion include:
| Elbow muscles | Flexors:
|
Extensors:
|
Pronation/Internal Rotation:
|
Supination/External Rotation:
|
|---|
Table 10.4 - Selected muscles of the elbow
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Biceps brachii |
|
Radial tuberosity |
|
Musculocutaneous nerve (C5-C6) | 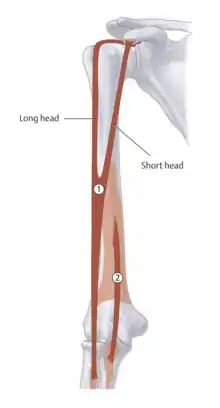 1 - Biceps brachii |
| Brachialis | Distal half of the anterior surface of the humerus; medial and lateral intermuscular septa | Ulnar tuberosity | Elbow flexion | Musculocutaneous nerve (C5-C6) and radial nerve (C7) | 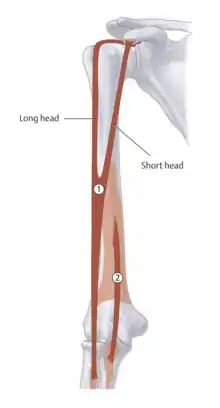 2 - Brachialis |
| Triceps brachii |
|
Olecranon of the elbow | Elbow extension; long head: shoulder backward movement and adduction | Radial nerve (C6-C8) | 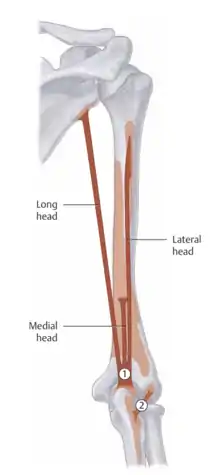 1 - Triceps brachii |
| Pronator teres |
|
Lateral surface of the radius |
|
Median nerve (C6-C7) | 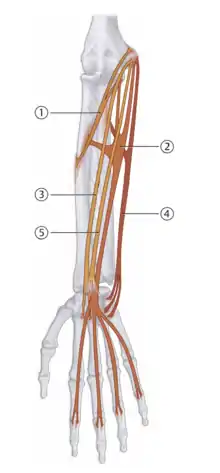 1 - Pronator teres |
Table 10.5 - Primary muscles of elbow and forearm motion
Motions that occur at the elbow are flexion, extension, supination, and pronation. Flexion and extension occur in the sagittal plane. The parallelogram effect describes pronation and supination having a reciprocal motion at the distal radius and the proximal radius (the radial head). During pronation, the radius rotates over the ulna; the distal radius moves anteriorly and medially, and the radial head moves posteriorly. During supination, the radius rotates and returns to its neutral position; the distal radius moves posteriorly and laterally, and the radial head moves anteriorly. Abduction and adduction occur in the coronal plane: in elbow abduction, the ulna abducts, moving laterally with respect to the humerus, the radius moves distally, and the carpal bones are pushed into adduction; in elbow adduction, the ulna adducts, moving medially with respect to the humerus, the radius moves proximally, and the carpal bones are pulled laterally. The carrying angle is an angle formed by the upper arm and the forearm with the forearm directed away from the body in a valgus position. A normal carrying angle is 10-15o in women and 5o in men. If the carrying angle is greater than 15o, this deformity is known as cubitus valgus; if the carrying angle is less than 15o, this deformity is known as cubitus varus.
Though the biceps brachii is the primary supinator of the forearm, the supinator muscle also contributes to this motion:
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Supinator | Olecranon, lateral epicondyle of humerus, radial collateral ligament, and annular ligament of the radius | Radius | Supinates the forearm | Radial nerve (C6-C7) | 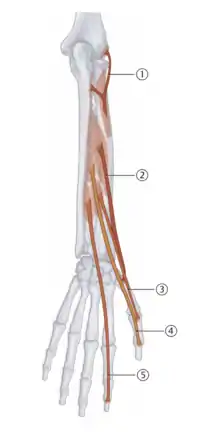 1 - Supinator |
Pathology affecting the elbow includes medial epicondylitis and lateral epicondylitis. Medial epicondylitis (“golfer’s elbow”) is characterized by pain near the ulnar groove involving the wrist flexors and the ulnar collateral ligament due to repetitive stress. Lateral epicondylitis (“tennis elbow”) is characterized by pain over the lateral epicondyle of the humerus involving the wrist extensors due to repetitive stress.
Elbow and Forearm Somatic Dysfunctions
Somatic dysfunction of the elbow is named for the motion that is present (i.e. ulnar abduction somatic dysfunction). Anterior radial head somatic dysfunctions occur most commonly from falling backward on an extended arm; posterior radial head somatic dysfunctions occur most commonly from a forward fall on an outstretched hand. The radial head is located by palpating the proximal lateral forearm; start by finding the olecranon and move laterally and distally. Supination and pronation of the arm can be used to locate it. When assessing for somatic dysfunctions of the radial head, one must compare both sides to identify the dysfunctional side.
| Example: Radial head somatic dysfunction diagnosis |
|---|
| A patient presents for evaluation of right elbow pain one week after he fell forward on an outstretched hand following a bicycle accident. This will result in a posterior radial head somatic dysfunction and demonstrate forearm supination restriction. (As discussed in the next section, the pronator teres muscle will be engaged when treating with a post-isometric relaxation muscle energy technique.) |
Treatment of Elbow and Forearm Somatic Dysfunctions
Treatment of somatic dysfunctions targets flexion and extension dysfunctions (relatively uncommon), anterior radial head dysfunction (also called supination dysfunction), posterior radial head dysfunction (also called pronation dysfunction), interosseous membrane restriction, and muscle group hypertonicity. Flexion and extension dysfunctions can be treated with direct post-isometric muscle energy. Radial head dysfunctions can be treated with either muscle energy or HVLA. Interosseous membrane restriction can be treated with myofascial release. Hypertonic muscles can be treated with counterstrain. Counterstrain for the elbow includes the short head of the biceps brachii/coracobrachialis, the supinator, and the pronator teres.
| Anterior Radial Head Post-Isometric Muscle Energy: The patient is seated. The physician contacts the dorsal aspect of the distal radius with the thumb. The other hand contacts the anterior and medial aspect of the radial head with the thumb. The patient is pronated to the restrictive barrier. The patient attempts supination against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Anterior Radial Head ME |
| Posterior Radial Head Post-Isometric Muscle Energy: The patient is seated and the physician grasps the patient's hand in a handshake fashion, contacting the palmar aspect of the distal radius with the index finger. The other hand contacts the posterolateral aspect of the radial head with the thumb. The patient is supinated to the restrictive barrier. The patient is attempts pronation against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Posterior Radial Head ME |
| Anterior Radial Head HVLA: The patient is seated. The physician holds the dysfunctional hand in a handshake fashion. The thumb of the other hand is placed anterior to the radial head. The physician pronates the forearm to the restrictive barrier. The physician carries the forearm into slight flexion and pronation while maintaining thumb pressure over the anterior radial head. |  Anterior Radial Head HVLA |
| Posterior Radial Head HVLA: The patient is seated. The physician holds the dysfunctional hand in a handshake fashion. The thumb of the other hand is placed posterior to the radial head. The physician supinates the forearm to the restrictive barrier. The physician carries the forearm into extension and supination while maintaining thumb pressure over the posterior radial head. |  Posterior Radial Head HVLA |
Myofascial release of the interosseous membrane can be performed for both the upper and lower extremities. The techniques are analogous and performed similarly:
| Interosseous membrane myofascial release: The physician palpates the forearm over the interosseous membrane and assesses for restrictions in range of motion in the three planes of motion (superior and inferior, left and right translation, and clockwise and counterclockwise rotation). After determining the ease/bind asymmetry, treatment can be performed directly or indirectly for 30-60 seconds. |  Interosseous Membrane MFR |
Counterstrain tenderpoints and treatments for selected upper extremity muscles:
| Tenderpoint+ | Location | Treatment position (initial setup) | Acronym | Figure (from Nicholas) |
|---|---|---|---|---|
| Supinator | Anterolateral aspect of the radial head at the attachment of the supinator | The patient is supine. The elbow is placed into full extension and the forearm is markedly supinated with a slight lateral (valgus) force | E Sup Val | 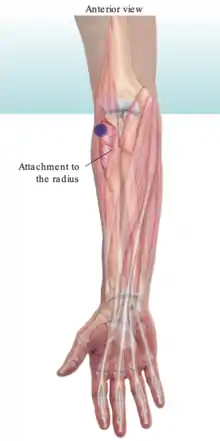 Supinator CS |
| Pronator teres | At or near the medial epicondyle of the humerus associated with common flexor tendon and the attachment of the pronator teres muscle | The patient is supine. The elbow is flexed, the wrist is pronated, and the forearm is slightly adducted. | F Pro Add |  Pronator Teres CS |
| Biceps brachii (short head) | At the inferolateral aspect of the coracoid process on the short head tendon of the biceps or the coracobrachialis muscle | The patient is supine. The elbow and shoulder are flexed and the shoulder is minimally internally rotated and abducted. | F Add IR | 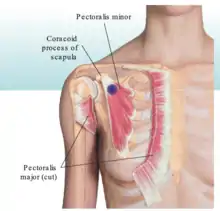 Pectoralis Minor CS |
| Pectoralis minor | Inferior and medial to the coracoid process | The patient is supine. The patient's arm is adducted across the chest and the scapula is pulled anteriorly, inferiorly, and medial | F Add |  Biceps Brachii CS |
+ Tenderpoints can be found anywhere along the length of the muscle; these are the most common tenderpoint locations.
Wrist and Hand Anatomy
There are 8 bones of the wrist: the scaphoid (sometimes called the navicular bone; this is the most commonly fractured wrist bone), which is the most lateral and proximal; the lunate (the second most commonly fractured carpal bone; the most commonly dislocated bone); the triquetrum; the pisiform (which is anterior to the triquetrum); the trapezium; the trapezoid; the capitate (largest of all the carpal bones); and the hamate.
The radius, scaphoid, lunate, and triquetrum comprise the true wrist. The head of the ulna is not part of the true wrist joint. Two axes of motion around which the wrist moves are a transverse axis (flexion/extension) and an anteroposterior axis (abduction/adduction).
The joints of the wrist and the hand include the radioulnar articulation, the radiocarpal joint, the midcarpal joint, the carpometacarpal joint, the metacarpophalangeal joint (the MCP joint), and the proximal and distal interphalangeal joint (the PIP and DIP joints). Motion at the wrist follows the restricted motion seen at the elbow. Elbow abduction occurs with wrist adduction; similarly, elbow adduction occurs with wrist abduction. These motions are termed reciprocal wrist motions.
The muscles of the wrist and hand are classified as extrinsic muscles and intrinsic muscles. The extrinsic muscles include the superficial flexors, the deep flexors, the superficial extensors, the deep extensors, and the radialis muscles. The intrinsic muscles include the thenar eminence, the hypothenar eminence, the lumbricals, the palmar interosseous muscles, and the dorsal interosseous muscles. (Table 10.5) The muscles of the thenar eminence are innervated by the recurrent branch of the median nerve and the muscles of the hypothenar eminence are innervated by the ulnar nerve. The palmar interosseous muscles participate in adduction and the dorsal interosseous muscles participate in abduction.
| Extrinsic muscles | Intrinsic muscles |
|---|---|
Superficial flexors:
|
Thenar eminence:
|
Deep flexors:
|
Hypothenar eminence:
|
Superficial extensors:
|
Lumbricals
|
Deep extensors:
|
Palmar interosseous muscles:
|
Radialis muscles:
|
Dorsal interosseous muscles
|
| Extensor carpi radialis (longus/brevis) |
|
|
|
Radial nerve (C6-C8) | 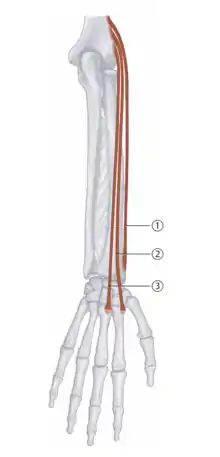 Extensor carpi radialis muscles: 2 - longus; 3 - brevis |
| Extensor carpi ulnaris | Lateral epicondyle of the humerus, ulnar head | Base of the fifth metacarpal | Extend, adduction/ulnar deviation | Radial nerve (C7-C8) | 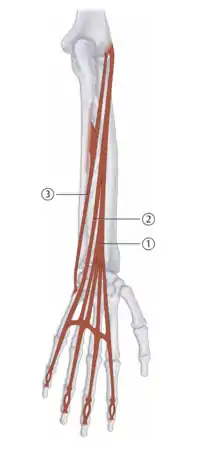 3 - Extensor carpi ulnaris |
| Flexor carpi radialis | Medical epicondyle of humerus | Base of the second metacarpal | Flexion and abduction/radial deviation of the hand | Median nerve (C6-C7) | 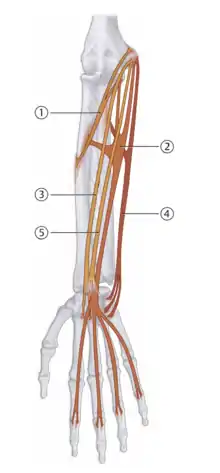 3 - Flexor carpi radialis |
| Flexor carpi ulnaris |
|
Pisiform hook of the hamate, base of the fifth metacarpal | Flexion and adduction/ulnar deviation of the hand | Ulnar nerve (C7-T1) | 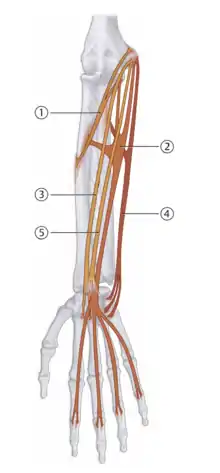 4 - Flexor carpi ulnaris |
Carpal tunnel syndrome is a common diagnosis involving the wrist and hand which arises from entrapment of the median nerve in the carpal tunnel; the structures which pass through the carpal tunnel include the tendons of the flexor digitorum profundus, the flexor digitorum superficialis, the flexor pollicis longus, and the median nerve. Due to impingement of the median nerve, paresthesias are experienced over the medial distribution of the hand (the thumb, the first two fingers and the medial half of the fourth digit).
Carpal tunnel syndrome can be assessed on physical exam using two provocative tests called Phalen’s test and Tinel’s test. Phalen’s test is done by the physician flexing the patient’s wrist as far as possible and holding for 60 seconds. The test is positive is paresthesias are reproduced. Tinel’s test is done by the physician tapping on the anterior surface of the transverse carpal ligament. A positive test will reproduce paresthesias expected in the median nerve distribution of the hand.
The tunnel of Guyon (sometimes stylized as Guyon’s canal) is a depression between the pisiform bone and the hook of the hamate; it contains the ulnar artery and the ulnar nerve.
The anatomic snuffbox is a triangular depression on the radial, dorsal aspect of the hand made by the scaphoid carpal bone (as the floor of the snuffbox), the abductor pollicis longus and the extensor pollicis brevis tendons on the radial border, and the extensor pollicis longus tendon on the ulnar border. DeQuervain’s tenosynovitis is an inflammation of the tendon and the tendon sheath secondary to repetitive use. It is characterized by pain with circumduction of the thumb. It can be tested for by using Finklestein’s test, during which the patient closes their fist around the thumb and ulnar deviates. The test is positive if pain is present at the anatomic snuffbox.
Two examples of hand injuries include the swan neck deformity and the boutonniere deformity. In the swan neck deformity, a flexion contracture is present at the metacarpophalangeal joint (abbreviated MCP) and the distal interphalangeal joint (abbreviated DIP), and an extension contracture is present at the proximal interphalangeal joint (abbreviated PIP). This results from a contracture of the intrinsic muscles of the hand. The boutonniere deformity is identified by an extension contracture of the MCP and the DIP, and a flexion contracture of the PIP. This occurs from rupture of the hood of the extensor tendon at the PIP. Both of these deformities are associated with rheumatoid arthritis.
Wrist and Hand Somatic Dysfunctions
Range of motion testing for the wrist should include flexion, extension, ulnar deviation (adduction), and radial deviation (abduction). Muscles that can cause extension dysfunctions of the wrist include extensor carpi ulnaris and extensor carpi radialis, among others. Muscles that can cause flexion dysfunctions of the wrist include flexor carpi ulnas and flexor carpi radialis, among others. Overuse of extensor muscles can lead to lateral epicondylitis. Muscles that flex the wrist are larger innervated by the median nerve and those that extend the wrist are innervated by the ulnar nerve.
Treatment of Wrist and Hand Somatic Dysfunctions
Myofascial release of the interosseous membrane was introduced in the prior section with Treatments of the Elbow and Forearm; it can be performed on the distal forearm in order to decompress the median nerve, increase the diameter of the carpal tunnel, increase shock absorption of the membrane, and prevent atrophy of the thenar eminence.
| Interosseous membrane myofascial release: The physician palpates the forearm over the interosseous membrane and assesses for restrictions in range of motion in the three planes of motion (superior and inferior, left and right translation, and clockwise and counterclockwise rotation). After determining the ease/bind asymmetry, treatment can be performed directly or indirectly for 30-60 seconds. |  Interosseous Membrane MFR |
Myofascial release of the flexor retinaculum:
| Flexor retinaculum release: The patient is seated. The patient's hand is placed in anatomical position. The physician's thumbs are placed over the medial and lateral attachments of the transverse carpal ligament. The fingers wrap around the dorsal surface of the wrist and exert pressure on the volar surface of the base of the band and spread apart, dragging the skin and superficial fascia with them. |  Flexor Retinaculum MFR |
Wrist range of motion somatic dysfunctions may be treated with post-isometric relaxation muscle energy:
| Wrist adduction somatic dysfunction: The physician abducts the patient's wrist to the restrictive barrier. The patient attempts to adduct the wrist against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Wrist Adduction Dysfunction ME |
| Wrist abduction somatic dysfunction: The physician adducts the patient's wrist to the restrictive barrier. The patient attempts to abduct the wrist against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Wrist Abduction Dysfunction ME |
| Wrist flexion somatic dysfunction: The physician extends the patient's wrist to the restrictive barrier. The patient attempts to flex the wrist against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Wrist Flexion Dysfunction ME |
| Wrist extension somatic dysfunction: The physician flexes the patient's wrist to the restrictive barrier. The patient attempts to extends the wrist against isometric resistance. During each iteration the patient is taken further into the restrictive barrier. |  Wrist Extension Dysfunction ME |
A dorsally-displaced carpal bone can be treated with HVLA:
| Dorsally-displaced carpal bone HVLA: The patient is seated. The physician grasps the dorsal aspect of the patient's wrist with one thumb over the other. The other fingers wrap around the palmar surface and the dorsally-dysfunctional carpal bone has pressure applied over it in a whipping motion. |  Carpal bone HVLA |
Counterstrain tenderpoints and treatments for selected upper extremity muscles:
| Tenderpoint+ | Location | Treatment position (initial setup) | Acronym | Figure (from Nicholas) |
|---|---|---|---|---|
| Extensor carpi radialis | Dorsal surface of the second metacarpal | The patient is seated or lays supine. The wrist if passively extended, abducted, and radially deviated | E Abd RD | 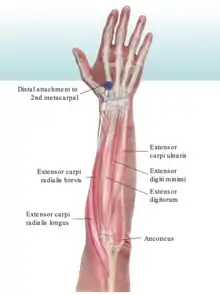 Extensor carpi radialis CS |
| Extensor carpi ulnaris | Dorsal surface of the fifth metacarpal | The patient is seated or lays supine. The wrist is passively extended, adducted, and ulnar deviation | E Add UD | 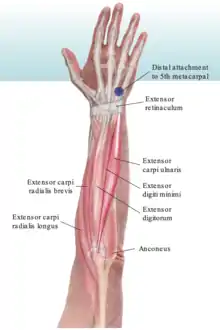 Extensor carpi ulnaris CS |
| Flexor carpi radialis | Palmar base of the second and third metacarpal | The patient is seated or lays supine. The wrist is passively flexed, abducted, and radially deviated | F Abd RD |  Flexor carpi radialis CS |
| Flexor carpi ulnaris | Palmar base of the fifth metacarpal | The patient is seated or lays supine. The wrist is passively flexed, adducted, and ulnar deviated | F Add UD |  Flexor carpi ulnaris CS |
Review Questions
1. A patient presents for evaluation of left elbow pain one week after he fell forward on an outstretched hand after tripping on the lip in a sidewalk. What muscle is to be utilized during post-isometric muscle energy for the dysfunction?
A. Supinator
B. Biceps brachii
C. Flexor carpi radialis
D. Flexor carpi ulnaris
E. Extensor carpi radialis
F. Extensor carpi ulnaris
G. Pronator teres
H. Pronator quadratus
2. A patient presents for evaluation of left elbow pain after stepping in a hole in his lawn and falling backward on his left hand. His likely somatic dysfunction is ____ with restriction in ____.
A. posterior radial head; forearm supination
B. posterior radial head; forearm pronation
C. anterior radial head; forearm supination
D. anterior radial head; forearm pronation
E. lateral epicondylitis; wrist flexion
F. lateral epicondylitis; wrist extension
G. medial epicondylitis; wrist flexion
H. medial epicondylitis; wrist extension
3. Consider the parallelogram effect and carrying angle of elbow and wrist motion. If the carrying angle were decreased, the ulna would deviate more ____, the radius would move ____, and the carpal bones would move ____.
A. laterally; inferiorly; medially
B. medially; inferiorly; medially
C. laterally; superiorly; medially
D. medially; superiorly; laterally
E. laterally; inferiorly; laterally
F. medially; inferiorly; laterally
4. A patient presents with restriction in wrist extension and the inability to flex the distal interphalangeal joint of the middle finger. Muscle strength testing, deep tendon reflexes, and sensation testing is unremarkable. Which muscle is most likely affected leading to these physical findings?
A. flexor digitorum superficialis
B. flexor digitorum profundus
C. flexor carpi ulnaris
D. flexor carpi radialis
E. flexor pollicis longus
5. A patient presents for evaluation of shoulder pain. She notes pain and restriction on internal rotation. Which rotator cuff muscle is most likely hypertonic leading to this somatic dysfunction?
A. the muscle that originates at the supraspinous fossa of the scapula and inserts on the superior facet of the greater tubercle of the humerus
B. the muscle that originates at the infraspinous fossa of the scapula and inserts on the middle facet of the greater tubercle of the humerus
C. the muscle that originates at the lateral border of the scapula and inserts on the inferior facet of the greater tubercle of the humerus
D. the muscle that originates at the subscapular fossa of the scapula and inserts on the lesser tubercle of the humerus
6. What is the initial setup for post-isometric relaxation muscle energy of a posterior radial head somatic dysfunction?
A. The physician contacts at the posterolateral aspect of the radial head and supinates the forearm until the restrictive barrier is reached. The patient attempts to pronate while the physician applies an isometric counterforce.
B. The physician contacts at the posterolateral aspect of the radial head and pronates the forearm until the restrictive barrier is reached. The patient attempts to supinate while the physician applies an isometric counterforce.
C. The physician contacts at the anteromedial aspect of the radial head and supinates the forearm until the restrictive barrier is reached. The patient attempts to pronate while the physician applies an isometric counterforce.
D. The physician contacts at the anteromedial aspect of the radial head and pronates the forearm until the restrictive barrier is reached. The patient attempts to supinate while the physician applies an isometric counterforce.
7. What is the initial setup for HVLA treatment of an anterior radial head somatic dysfunction?
A. The physician contacts the proximal radial head and rotates the forearm until into supination until the restrictive barrier is reached. The physician carries the forearm into slight extension and supination while maintaining thumb pressure over the anterior radial head.
B. The physician contacts the proximal radial head and rotates the forearm until into pronation until the restrictive barrier is reached. The physician carries the forearm into slight flexion and pronation while maintaining thumb pressure over the anterior radial head.
C. The physician contacts the proximal radial head and rotates the forearm until into pronation until the restrictive barrier is reached. The physician carries the forearm into slight extension and supination while maintaining thumb pressure over the anterior radial head.
D. The physician contacts the proximal radial head and rotates the forearm until into supination until the restrictive barrier is reached. The physician carries the forearm into slight flexion and pronation while maintaining thumb pressure over the anterior radial head.
8. Which of the following is not an objective of myofascial release of the interosseous membrane?
A. Decompress the median nerve
B. Increase the diameter of the carpal tunnel
C. Increase shock absorption of the membrane
D. Relieve compression of the ulnar nerve
E. Prevent atrophy of the thenar eminence
9. Atrophy of the thenar eminence is caused by injury to the ____ nerve; atrophy of the hypothenar eminence is caused by injury to the ____ nerve.
A. radial; ulnar
B. radial; median
C. median; radial
D. median; ulnar
E. ulnar; radial
F. ulnar; median
10. Which of the following muscles does not attach to the scapula?
A. Biceps brachii
B. Rhomboid major
C. Brachioradialis
D. Coracobrachialis
E. Trapezius
11. A 25-year-old female presents for evaluation of left forearm and wrist pain for the last week. She denies any trauma. She is a professional tennis player and has been practicing more frequently for upcoming matches. She denies any paresthesias. Her medical history is unremarkable. Her vital signs are stable. Muscle strength testing, deep tendon reflexes, and sensation testing are unremarkable. She notes tenderness when palpated at the lateral humerus. What is the initial counterstrain setup for a tenderpoint associated with the hypertonic muscle which muscle originates at the lateral humerus and inserts at the base of the second metacarpal causing her symptoms?
A. Flexion and radial deviation
B. Flexion and ulnar deviation
C. Extension and radial deviation
D. Extension and ulnar deviation
12. A 55-year-old male presents to the office with a complaint of right shoulder pain that began 2 weeks ago and has been progressively getting worse. He reports some radiation of the pain into the neck but denies any numbness or tingling. Past medical history is significant for diabetes mellitus type 2. Vital signs are unremarkable. Physical exam reveals muscle strength of 5/5 and deep tendon reflexes of 2/4 in the bilateral upper extremities. Structural examination reveals:
- Preference for internal rotation of the right shoulder
- OA ESRRL
- T2-T4 NSRRL
- T7 ESLRL
- L1-L2 NSRRL
- Positive seated flexion test on the left; deep sacral sulcus on the left; deep ILA on the left
To treat this patient's shoulder somatic dysfunction with muscle energy, the patient's activating force is provided by which of the following muscles?
A. Teres minor
B. Latissimus dorsi
C. Pectoralis minor
D. Rhomboid major
E. Triceps brachii
13. A patient with a history of rheumatoid arthritis presents for evaluation of intractable hand pain. She is noted to have a flexion contracture of the MCP and DIP joints and an extension contracture at the PIP joint secondary to contracture of the intrinsic muscles of the hand. What is the name of this constellation of contractures? (Note: Though introduced in this chapter, further information regarding the neuroanatomical basis and mechanism for this deformity can be found in Chapter 13.)
A. swan neck deformity
B. boutonniere deformity
C. claw hand
D. wrist drop
E. Klumpke's palsy
F. ape hand
Answers to Review Questions
- G
- D
- D
- B
- B
- A
- B
- D
- D
- D
- C
- A
- A