Chapter 7: Innominates, Hip, and Pelvis
Objectives:
- To identify the primary muscles that flex and extend the hip, adduct and abduct the hip, and internally and externally rotate the hip
- Explain how the iliolumbar ligament, anterior sacral ligament, sacrospinous ligament, and sacrotuberous ligament affect the sacrum, innominates and lumbar spine
- Identify and treat somatic dysfunction of the innominates based on landmark findings using the standing flexion test, seated flexion text, ASISs, PSISs, and medial malleoli
- Diagnose pubic shears as well as piriformis and psoas hypertonicity and respective counterstrain tenderpoints.
Innominate, Hip, and Pelvis Anatomy
The innominate (“no name”) is comprised of three separate bones that fuse early in life to form the acetabulum (hip socket) where the femur articulates with the hip bones: the ilium (flank) is the most superior and the largest, the ischium (flank) forms the inferior and posterior part of the bone, and the pubis (groin) is the inferior and anterior part of the bone. There are differences between the male and female genders with regard to the anatomic structure of the pelvis. The suprapubic angle is acute in males and obtuse in females.
The following structures serve as important landmarks of the anterior pelvis and as attachment sites of ligaments and muscles: the iliac crest, which is at the level of L4, the anterior superior iliac spine (ASIS), the anterior inferior iliac spine (AIIS), the pubic symphysis, where the innominates join together, and the ischial ramus. Recall that these landmarks are also the site of the lumbar counterstrain tenderpoints.
The following structures serve as important landmarks in addition to those on the anterior surface: the posterior superior iliac spine (PSIS), the posterior inferior iliac spine (PIIS), the ischial tuberosity, the iliac crest, the ilium, and the pubis. Posteriorly, the acetabulum cannot be seen because of the forward-angling of the site of insertion of the femur.
There are two major joints that join the bones of the pelvis together: the pubic symphysis, a dense fibrous cartilage that joins the two pubis bones together, and two sacroiliac joints, which connect the sacrum to the innominates. Collectively, these structures make up the pelvis. There are four important ligaments to identify when considering pelvis anatomy: the iliolumbar ligament is a broad ligament that stabilizes L5 and anterior motion of the lower lumbar spine; the anterior sacral ligament (or sacroiliac ligament) connects the sacrum to the innominates; the sacrospinous ligament connects the sacrum to the ischial spine; and, the sacrotuberous ligament which connects the sacrum to the ischium. The sacrospinous and sacrotuberous ligaments restrict sacral flexion and posterior innominate rotation. The sacroiliac ligament is contiguous with the sacrotuberous ligament. The significance of these ligaments is that the sacrum is intricately connected through each of the three bones that make up the innominate. Therefore, dysfunctions of either one will likely have an impact on the other.
The muscles of the hip can be classified as shown below in Table 7.1. Any hypertonicity in these muscles will result in somatic dysfunction of the innominate.
| Hip Flexors | Hip Extensors | Hip Adductors | Hip Abductors | Hip External Rotators |
|---|---|---|---|---|
|
|
|
|
|
Note:
- Three muscles of the quadriceps (vastus laterals, vastus medialis, and vastus intermedius actually attach to the femur and function more as knee extensors than hip flexors.
- The rectus femoris serves more as a hip flexor due to its attachment to the ilium.
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Psoas (psoas major; part of Iliopsoas) | T12-L4 vertebral bodies | Lesser trochanter of the femur |
|
Femoral nerve and lumbar plexus | 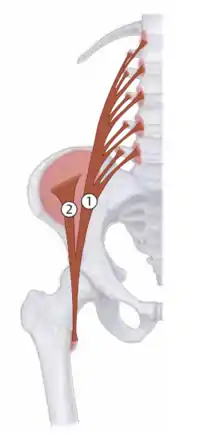 Iliopsoas: 1 - Psoas major |
| Piriformis | Anterior surface of the sacrum | Greater trochanter of the femur | Hip: external rotation, abduction, and extension | Sacral plexus (L5-S2) | 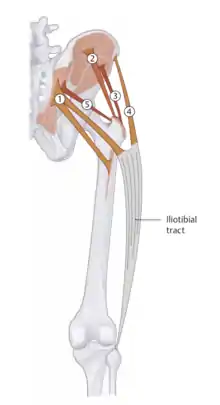 5 - Piriformis |
The psoas and piriformis muscles are major contributors to low back pain causes. The piriformis muscle is the primary external rotator of the lower extremities. The sciatic nerve exits from the lumbosacral plexus and usually passes below the piriformis but, in approximately 10% of cases, it passes through the piriformis (known as piriformis syndrome). Therefore, with a hypertonic piriformis muscle, sciatic nerve pain may be a presenting symptom of low back pain. The piriformis is also the only muscle that connects to the sacrum as well as being the only muscle on the anterior surface of the sacrum. Piriformis function depends on the position of the hip – if the hip is flexed, it acts more as an abductor; if extended, where it acts more as an external rotator.
The FAIR test (Flexion, Adduction, and Internal Rotation) is used to detect a hypertonic piriformis. The test is considered positive if pain is felt in the gluteal region while the test is being performed.
If a patient experiences a hypertonic psoas muscle, one would expect the lumbar spine, based on the attachments of the muscle, to be sidebent ipsilaterally and contralaterally rotated as this would create a type 1 dysfunction affecting multiple vertebrae (T12-L4). Also observed would be a preference for ipsilateral hip flexion. Psoas syndrome is characterized by a pattern of somatic dysfunction of the low back and hip which centers around a hypertonic psoas muscle on one side, causing sidebending of the lumbar spine to that side, shortening of the ipsilateral leg, and eversion of the ipsilateral foot as well as a tight piriformis on the contralateral side leading to external rotation of the contralateral leg and sciatica as described in the last paragraph. The pain pattern is usually in the thoracolumbar junction and the anterior medial thigh on the ipsilateral side as the tight psoas. The contralateral side with the piriformis spasm will have pain in the buttocks from the inferior lateral angle of the sacrum to the greater trochanter of the femur and into the posterior and lateral thigh usually to the level of the knee but not below.
The Thomas test is used to diagnose psoas hypertonicity. It is done by having the patient lay supine and bring both knees to the chest. Upon straightening the leg to be tested, if the knee remains involuntarily flexed, the test is positive. (Some patients with psoas syndrome may not be able to tolerate this. A modified Thomas test can be used where the patient has their legs hanging off the table and the knee is brought to the chest.)
With psoas dysfunctions, the top segment of attachment (L1) will show a type 2 dysfunction and the remainder of the segments (L2-L4) will show type 1 dysfunctions. Additionally, it is seen that the opposite piriformis and psoas muscles are hypertonic to compensate.
| Example: Hypertonic psoas/piriformis relationship |
|---|
| If the right psoas muscle is hypertonic, the left piriformis muscle will also be hypertonic as compensation. |
Additional tests used in the Osteopathic Structural Exam are detailed in Chapter 1.
The pelvic girdle is made of the two innominates and the sacrum. There are differences in the angles between the android male pelvis (acute, ca. 70o) and the gynecoid female pelvis (obtuse, ca. 100o). The gynecoid pelvis has increased flaring of the ilia. The android pelvis is heavier and has more pronounced muscle attachment; the ischial tuberosities are closer in the android pelvis than in the gynecoid pelvis, and the pelvis outlet is thus comparatively smaller. All of the ilia are less flared in the android pelvis than in the gynecoid pelvis, so the greater pelvis is deeper. The pelvic inlet is heart-shaped in the android pelvis and more transversely oval in the gynecoid pelvis. The gynecoid pelvis is broader than in the android pelvis to allow the passage of the fetal head.
The pelvic diaphragm (interchangeably called the pelvic floor) is often overlooked as a source of pain. It may be the cause of lower back pain but is not often considered as the first issue. It serves as a major crossroads for blood, lymph, and nerves and is closely connected to the abdominal diaphragm. Most dysfunctions of the pelvic diaphragm occur in females during pregnancy. The muscles of the pelvic diaphragm include the levator ani (composed of the puborectalis, the pubococcygeus, and the iliococcygeus) and the coccygeus. The piriformis and the coccygeus form the posterolateral aspects of the pelvic floor. The ischial tuberosity serves as a landmark for treating pelvic floor dysfunctions. To contact the pelvic diaphragm, the physician will palpate through a significant amount of connective tissue and adipose. Once a firm feeling is palpated, contact is made. The pelvic diaphragm will move with the respiratory cycle and tighten with inspiration.
The pubic symphysis is a dense fibrocartilaginous joint. Under physiologic conditions, the pubic tubercles should be less than 1 cm apart; the symphysis has the inherent ability to move ca. 2 mm superiorly or inferiorly during the gait cycle. Rotation is limited to 1-2o. The major function of the pubic symphysis is force distribution. During pregnancy, the pubic symphysis becomes relaxed.
Innominate, Hip, and Pelvis Somatic Dysfunctions
Somatic dysfunctions of the innominate can be classified as a rotation somatic dysfunction, a shear somatic dysfunction, or a flare somatic dysfunction. The static findings of the innominate landmarks are used to diagnose somatic dysfunctions. (Table 7.2)
| The standing flexion test lateralizes somatic dysfunction of iliosacral motion. The patient stands with their knees extended and feet apart at a distance equivalent to the positions of the acetabulum. The physician sits behind the patient with eyes at the level of the patient’s posterior superior iliac spine (PSIS). The patient is asked to bend forward slowly without flexing their knees. During the bending motion, the physician will observe anterosuperior excursion of thumbs on the patient’s PSIS and note if one side moves further than the other. The side that moves first and moves the furthest is the positive side, indicating iliosacral restriction of the ipsilateral side. The SI (sacroiliac) compression test (or ASIS compression test) is done with the patient in a supine position. The physician places their palms bilaterally over the patient’s anterior superior iliac spine (ASIS). The physician then presses posteriorly and laterally. The test is positive on the side with a lack of motion. Both the standing flexion test and the SI compression test can be used to diagnose innominate and sacral somatic dysfunctions. |  Standing flexion test |
Innominate diagnosis can be made using a pelvic lateralization test followed by examining pelvic landmarks. Pelvic lateralization tests include the standing flexion test and the ASIS compression test. The lateralization test helps to determine the dysfunctional side only, not the direction of dysfunction. To determine which direction the dysfunction is occurring, the position of the ASIS, PSIS, and relative leg lengths must be assessed.
- ASIS: The relative position of the ASIS should be evaluated with the patient supine, taking care to keep the dominant eye level and centered with the patient’s body. The ASIS positions from superior to inferior should be level with one another. If the heights are unlevel, this could indicate an anterior or posterior rotation of the innominate on the dysfunctional side. This finding could also indicate a superior or inferior shear of the innominate. Evaluating the PSIS will make this determination. The ASIS should also be compared for medial/lateral position with respect to the midline to evaluate for possible flaring of the innominate. The midline landmark usually used is the umbilicus, although the pubic symphysis or xiphoid process are also acceptable. Keep in mind that if the patient has had abdominal surgery, the umbilicus may not be an accurate representation of midline.
- PSIS: The relative position of the PSIS should be evaluated with the patient prone, taking care to keep the dominant eye level and centered with the patient’s body. The PSIS positions from superior to inferior should be level with one another. If the heights are unlevel in the opposite direction from the ASIS, then the patient has a rotation dysfunction of the innominate. If the heights are unlevel in the same direction as the ASIS, then the patient has a shear dysfunction of the innominate.
- Leg lengths: Evaluating the relative length of the lower extremities, while not necessary to make an innominate diagnosis, is a helpful tool to confirm pelvic findings. Leg length evaluation is done with the patient in the supine position.
Before landmark assessment can be done, the patient must first contract and relax all muscles attached to the innominates to ensure that muscle imbalances are not causing false positives. This process is called resetting the pelvis and is done by:
- asking the patient to flex their knees
- actively lift their trunk off the table
- actively return their trunk to the table
- and then passively extending their knees back the supine position
 Resetting the Pelvis |
Once the pelvis is reset, the medial malleoli positions are evaluated relative to one another to determine a rough estimate of leg length. Under typical conditions, the leg lengths should mirror the findings of the ASIS (i.e. if the right ASIS is inferior compared to the left, then the right medial malleolus should also be inferior to the left). Similarly, if the innominate dysfunction is treated, then the leg lengths should return to equal. If the innominates are treated and pelvic landmarks are equal, but leg lengths remain unequal, then the patient is likely to have a congenital leg length discrepancy.
Based on the landmark findings, the following chart (Table 7.2) will help establish an innominate somatic dysfunction. Remember that the noted positions are with respect to the dysfunctional side as determined by the lateralization test.
| Diagnosis | Relative ASIS position | Relative PSIS position | Relative leg length | Hypertonic muscle |
|---|---|---|---|---|
| Anterior rotation | Lower | Higher | Longer on affected side | Quadriceps |
| Posterior rotation | Higher | Lower | Shorter on affected side | Hamstrings |
| Superior shear | Higher | Higher | Shorter on affected side | |
| Inferior shear | Lower | Lower | Longer on affected side | |
| Inflare | Medial* | Lateral* | Even leg lengths | |
| Outflare | Lateral* | Medial* | Even leg lengths |
An anterior innominate somatic dysfunction would be caused by hypertonic quadriceps muscles as the innominate is being pulled forward (i.e. flexed) around the inferior transverse axis of the sacrum. Note that superior shears closely resemble posterior innominate dysfunctions except for leg lengths; the same is true for inferior shears with anterior dysfunctions. To assess for an inflare or outflare dysfunction, the relative positions of the ASIS and the umbilicus are compared.
| Example: Innominate somatic dysfunction diagnosis |
|---|
| For a patient who demonstrates a standing flexion test that is positive on the right, a negative seated flexion test, a PSIS that is lower on the right, and an ASIS that is lower on the left, the diagnosis is a right posterior rotation innominate somatic dysfunction. First, the standing flexion test is used to lateralize the dysfunction to the right side, so all landmarks should be judged relative to the right side. The PSIS is found to be lower on the right. The ASIS is found to be lower on the left, meaning that it is higher on the right. Leg lengths are not provided. Using this information, the side with the lower landmark is used to diagnose the rotation somatic dysfunction. A posterior rotation dysfunction is caused by hypertonic hamstring muscles, since the innominate is pulled backward (i.e. extended). |
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Quadriceps femoris |
|
Tibial tuberosity (via patellar ligament) |
|
Femoral nerve (L2-L4) | 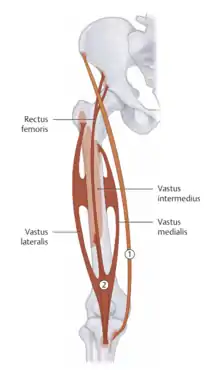 Quadriceps femoris muscles: vastus medialis, vastus lateralis, vastus intermedia, rectus femoris |
| Hamstrings |
|
|
|
Tibial nerve (L5-S2) | 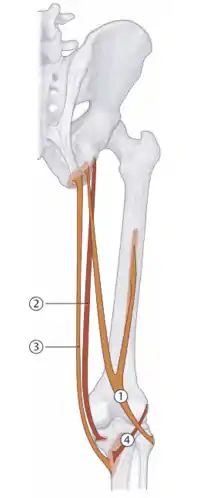 Hamstrings: 1 - Biceps femoris, 2 - Semimembranosus, 3 - Semitendinosus |
Treatment of Innominate Somatic Dysfunctions
Rotation dysfunctions (i.e. anterior and posterior innominate somatic dysfunctions) may be treated with post-isometric relaxation muscle energy and HVLA techniques:
| Anterior Innominate Rotation Post-isometric Relaxation Muscle Energy: The patient may be either prone or supine. The physician is positioned to the side of the table on the dysfunctional side. With one hand monitoring the PSIS, passively flex the hip until motion is felt in the innominate. Ask the patient to extend their hip, and resist their force to create an isometric contraction. | 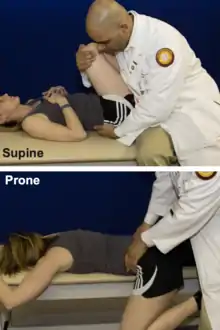 Anterior Innominate Muscle Energy |
| Posterior Innominate Rotation Post-isometric Relaxation Muscle Energy: The patient may be either prone or supine. The physician is positioned to the side of the table on the dysfunctional side. With one hand monitoring the PSIS, passively extend the hip until motion is felt in the innominate. Ask the patient to flex their hip, and resist their force to create an isometric contraction. |  Posterior Innominate Muscle Energy |
| Anterior Innominate Rotation HVLA: The patient is lateral recumbent on the affected side with legs flexed until motion is felt at the level of L5-S1. The lower leg is dropped off the side of the table without the foot touching the floor. The physician places the caudad forearm between the patient’s PSIS and trochanter and the cephalad hand is placed on the patient’s left shoulder. The force vector is directed down the leg once the barrier is approximated. |  Anterior Innominate HVLA |
| Posterior Innominate Rotation HVLA: The patient is lateral recumbent on the affected side with legs flexed until motion is felt at the level of L5-S1. The lower leg is straightened, and the foot on the higher leg is tucked into the contralateral popliteal fossa. The physician’s forearm contacts the iliac crest, and a rotational thrust with a force vector toward the physician’s umbilicus is applied once the barrier is reached. |  Posterior Innominate HVLA |
Flare dysfunctions can be treated with post-isometric relaxation muscle energy:
| Inflare Innominate Post-isometric Relaxation Muscle Energy: The patient is in the supine position. The physician is positioned to the side of the table on the dysfunctional side. With one hand stabilizing the ASIS on the opposite side, passively flex the hip to 90 degrees and abduct the hip to the restrictive barrier. Ask the patient to adduct their hip, and resist their force to create an isometric contraction. |  Inflare Innominate Muscle Energy |
| Outflare Innominate Post-isometric Relaxation Muscle Energy: The patient is in the supine position. The physician is positioned to the side of the table on the dysfunctional side. With one hand firmly grasping the PSIS on the dysfunctional side, passively flex the hip to 90 degrees and adduct the hip to the restrictive barrier. Ask the patient to abduct their hip, and resist their force to create an isometric contraction. Simultaneously pull laterally on the PSIS while the patient is contracting. |  Outflare Innominate Muscle Energy |
Shear dysfunctions can be treated with muscle energy and HVLA techniques:
| Superior Innominate Shear HVLA: The patient is in the supine position. The physician is positioned at the foot of the table. Firmly grasp the tibia/fibula of the dysfunction-side lower extremity, and internally rotate the lower extremity until the innominate starts to rise off the table. Apply traction to the lower extremity until reaching the innominate restrictive barrier. Ask the patient to forcibly cough and apply a tractional thrust. |  Superior Shear HVLA |
| Inferior Innominate Shear Post-Isometric Relaxation Muscle Energy: The patient may be either prone or supine. The physician is positioned to the side of the table on the dysfunctional side. With one hand firmly contacting the ischial tuberosity on the dysfunctional side, passively flex the hip until motion is felt in the innominate. Ask the patient to extend their hip, and resist their force to create an isometric contraction. Simultaneously apply superior pressure onto the ischial tuberosity as the patient contracts. |  Inferior Shear Muscle Energy |
Hypertonic psoas and piriformis muscles can be treated with counterstrain, post-isometric relaxation muscle energy, and reciprocal inhibition muscle energy techniques.
Counterstrain:
| Tenderpoint | Location | Treatment position (initial setup) | Acronym | Figure |
|---|---|---|---|---|
| Psoas | Anteriorly 2/3 of the distance from the ASIS to the umbilicus (midline) | Patient is supine. Flex the hips and knees with added slight external rotation of the hips and pulling of the knees toward the tenderpoint to sidebend the lumbar spine. | F ST ER | 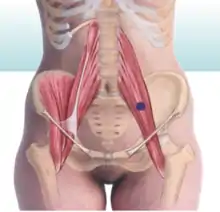 Psoas Tenderpoint |
| Piriformis | Posteriorly midpoint between the lower half of the lateral aspect of the sacrum and inferolateral angle and the greater trochanter | Patient is prone. Flex, abduct, and externally rotate the dysfunction-side lower extremity. | F Abd ER |  Piriformis Tenderpoint |
Hypertonic psoas and piriformis muscle energy techniques:
| Post-isometric relaxation muscle energy of a hypertonic psoas muscle | The patient lies prone and the physician flexes the patient's knee on the dysfunctional side to 90 degrees, grasping the thigh just above the knee. The physician's other hand stabilizes the pelvis by applying a gentle pressure over the sacrum. The physician lifts the patient's knee to the restrictive barrier and instructs the patient to pull their knee down toward the table. The physician resists with an isometric force. |  Psoas PIR ME |
|---|---|---|
| Reciprocal inhibition muscle energy of a hypertonic psoas muscle | The patient lies supine at the end of the table with the dysfunctional lower extremity hanging off the table. The non-dysfunctional hip is flexed by bringing the hip to the chest to flatten the lumbar lordosis. The physician positions the patient's thigh toward the floor extending the hip into the restrictive barrier. The physician instructs the patient to push down toward the floor while the physician resists. The physician brings the patient further into the barrier. |  Psoas RI ME |
| Post-isometric relaxation muscle energy of a hypertonic piriformis muscle | The patient lies supine. The hip and knee are flexed so that the foot on the dysfunctional side is placed lateral to the unaffected knee. The cephalad hand is placed on the ASIS on the side of the hypertonic muscle to stabilize the pelvis. The caudad hand pulls the affected knee toward the midline, internally rotating the hip, until the restrictive barrier is engaged. The patient pushes toward the midline while the physician resists. The physician brings the patient further into the barrier. |  Piriformis PIR ME |
| Reciprocal inhibition muscle energy of a hypertonic piriformis muscle | The patient lies prone. The physician palpates the hypertonic piriformis muscle with one hand and grasps the patient's ankle, flexing the knee to 90 degrees and internally rotating the ankle until the restrictive barrier is reached. The patient is instructed to bring the ankle toward the midline while the physician resists. The physician brings the patient further into the barrier. |  Piriformis RI ME |
Spencer's technique is used to evaluate the hip and can be used as both a diagnostic test and can be converted into a muscle energy or articulatory treatment. The goals of the Spencer technique are to improve hip mechanics and range of motion, stretch local tissues, improving lymphatic flow, and to improve circulatory flow.
The stages are:
| Flexion | Knee flexion takes the hip to the flexion extension barrier |  Spencer's technique of the hip - flexion |
|---|---|---|
| Extension | Knee is extended off the table |  Spencer's technique of the hip - extension |
| Circumduction with compression | Flexion of the hip with compression and circular movement in both clockwise and counterclockwise fashion |  Spencer's technique of the hip - circumduction with compression |
| Circumduction with traction | Extension of the knee; grasp the foot and ankle with traction and rotate the hip through increasingly large circles in both clockwise and counterclockwise fashion |  Spencer's technique of the hip - circumduction with traction |
| Internal rotation | Flex the hip and flex the knee while internally rotating the hip to its barrier |  Spencer's technique of the hip - internal rotation |
| External rotation | Flex the hip and flex the knee while externally rotating the hip to its barrier |  Spencer's technique of the hip - external rotation |
| Abduction | With the leg straight, it is taken to its abduction barrier |  Spencer's technique of the hip - abduction |
| Adduction | With the leg straight, it is taken to its adduction barrier |  Spencer's technique of the hip - adduction |
Spencer's technique can be converted into an articulatory technique or a post-isometric muscle energy technique if a barrier is appreciated. Following treatment, the dysfunction is reassessed in the same way that it was initially assessed. Be sure to correctly diagnose the somatic dysfunction and, if treating with a direct technique such as muscle energy, the appropriate restrictive barrier is engaged.
| Treating Spencer's technique somatic dysfunctions |
|
|---|
Spencer’s technique has an analogous sequence for the shoulder and this will be discussed in Chapter 10.
Review Questions
Questions 1-7: Match the innominate diagnosis based on the following static findings (choices may be used more than once):
1. Positive ASIS compression test on the right. Seated flexion test is negative. Left PSIS is lower than that on the right. ASIS is lower on the right compared to the left.
2. Positive standing flexion test on the right. Seated flexion test is negative. Left PSIS is higher than that on the right. ASIS is higher on the right compared to the left.
3. Closely resembles a right inferior pubic shear.
4. Positive ASIS compression test on the left. Seated flexion test is negative. Right ASIS is lower than that on the left. Left PSIS is lower compared to the right. The right leg is longer than the left leg.
5. Positive standing flexion test on the right. Seated flexion test is negative. Right ASIS is superior compared to that on the left. Left PSIS is inferior compared to that on the right.
6. Positive standing flexion test on the left. Right ASIS is higher than that on the left. Left PSIS is higher than that on the right.
7. Positive ASIS compression test on the left. Left ASIS is medially located. Right PSIS is medially located.
A. Right anterior innominate
B. Right posterior innominate
C. Left anterior innominate
D. Left posterior innominate
E. Right inflared innominate
F. Right outflared innominate
G. Left inflared innominate
H. Left outflared innominate
I. Right superior innominate shear
J. Right inferior innominate shear
K. Left superior innominate shear
L. Left inferior innominate shear
8. A patient presents for evaluation of left leg pain. She notes that she intermittently experiences a shooting pain down the back of her left leg to the knee. When examined supine, her left leg is externally rotated. What nerve is most likely irritated causing her leg pain?
A. Obturator nerve
B. Fibular nerve
C. Femoral nerve
D. Sciatic nerve
E. Direct branches from the sacral plexus (L5-S2)
10. An anterior innominate somatic dysfunction is caused by a hypertonic ____ muscle and a posterior innominate somatic dysfunction is caused by a hypertonic ____ muscle.
A. hamstrings; hamstrings
B. hamstrings; quadriceps
C. quadriceps; hamstrings
D. quadriceps; quadriceps
11. Where would a tenderpoint be expected to be found for a left hypertonic psoas muscle?
A. Left greater trochanter
B. Left lesser trochanter
C. Right greater trochanter
D. Right lesser trochanter
12. What is the initial setup for the treatment of a hypertonic piriformis muscle using counterstrain with the patient supine?
A. Hip is flexed, adducted, and externally rotated
B. Hip is flexed, abducted, and externally rotated
C. Hip is extended, abducted, and internally rotated
D. Hip is extended, adducted, and externally rotated
E. Hip is flexed, abducted, and internally rotated
F. Hip is extended, abducted, and externally rotated
Answers to Review Questions
- A
- B
- A
- D
- I
- C
- G
- D
- C
- C
- B