Chapter 15: Additional Treatment Techniques
Objectives:
- Describe the basis and mechanism of Balanced Ligamentous Tension (Ligamentous Articular Strain) techniques
- Describe the basis and mechanism of Facilitated Positional Release techniques
- Describe the basis and mechanism of Still techniques
Overview of Treatment Techniques
| Technique | Direct or indirect | Active or passive | Mechanism of action | Absolute contraindications | Relative contraindications |
|---|---|---|---|---|---|
| Balanced Ligamentous Tension (Ligamentous Articular Strain) | Direct or indirect | Passive |
|
|
|
| Facilitated Positional Release | Indirect | Passive | Muscle spindle fibers return to normal length decreasing tension in muscle activity fibers |
|
|
| Still's Technique | Indirect | Passive | Indirect positioning toward the ease of somatic dysfunction in which pressure is applied followed by a another part of the body being used as a long-levered force vector to move the segment through the least resistant path toward the barrier causing relaxation of hypertonic musculature |
|
|
Balanced Ligamentous Tension
Balanced Ligamentous Tension (also used interchangeably with Ligamentous Articular Strain) is performed by moving the dysfunctional segment into a position of ease, adding an appropriate amount of compressive activating force, and while maintaining compression, using moderate acceleration to move the segment towards the restrictive barrier. Following treatment, the compression is slowly released before the restrictive barrier is fully engaged, and return the patient to neutral. The patient is reassessed in a neutral position. Duration of treatment is typically 30 seconds.
Summarizing:
- Disengage the area of somatic dysfunction using compression or traction
- Exaggerate the ease
- Balance the ease and restrictive forces for 30 seconds
- Reassess
| Spinal Sacral Tethering Emphasis: The patient lies supine. The physician places their hand under the sacrum such that the finger pads are at the sacral base and the heel of the hand is toward the coccygeal region. The other hand is placed at the lvel of the dysfunctional segment such that the heel of the hand and finger pads contact the left and right L5 transverse processes. The hand on the sacrum evaluates ease/bind of the sacrum between flexion and extension. The lumbar hand sidebends and rotates L5 to a point of balanced tension. |  Spinal Sacral Tethering Emphasis BLT |
| Posterior Fibular Head Dysfunction: The patient is supime. The hip and knee are flexed to 90 degrees. The physician's thumb is placed at the superolateral aspect of the fibular head. The other hand controls the foot just inferior to the distal fibula. The thumb adds pressure on the proximal fibula directed toward the foot as the other hand inverts the foot and ankle until a point of balanced tension is achieved. |  Posterior Fibular Head BLT |
| Cruciate Ligament Sprain: The patient is supine. The physician places one pal over the anterior distal femur and the other pal over the tibial tuberosity. The physician adds a compressive force to approximate the femur and the tibia, followed by internal and external rotation to achieve a point of balanced tension. |  Cruciate Ligament Sprain BLT |
| Posterior Tibia on Talus: The patient is supine. The physician places their palm across the distal tibia with the MCP joint of the index finger proximal to the distal tibia. the physician presses downward and then uses the other hand on top of the hand on the distal tibia and assesses internal and external rotation by applying more pressure until a point of balanced tension is achieved. |  Posterior Tibia on Talus BLT |
| Boot Jack (Left Calcaneus Plantar Flexion): The patient is supine. The patient's lower thigh and knee are placed under the physician's contralateral axilla and lateral rib cage. The patient grasps the dysfunctional calcaneus with the thumb and index finger. The dysfunctional hip and knee are flexed to 90 degrees and externally rotated. The physician's distal humerus and elbow contact the distal femur to generate proximal pressure. The foot is plantarflexed and the hips and knees flexed until a point of balanced tension is reached. | 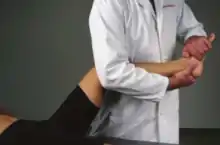 Boot Jack BLT |
Facilitated Positional Release
Facilitated Positional Release (FPR) is a passive and indirect technique that is performed by appropriately flexing or extending the spine to flatten the anteroposterior curve at the area to be treated. A gentle axial compressive force (one pound or less) is applied. While maintaining neutralization of the spinal curve and activating compressive force, the dysfunctional segment is moved into flexion or extension to increase ease of motion and into sidebending and rotational ease of motion. This position is held for 3-5 seconds. The compression is released and the patient is returned to neutral. The somatic dysfunction is reassessed in neutral position for improvement.
| Cervical Spine FPR: The patient lies supine. The physician supports the head with the hand on the same side as the prominent articular pillar. The cervcal spine is neutralized with a slight flexion followed by the application of an activating force in the form of a gentle axial compression while the patient's head is positioned toward the dysfunction for 3 to 5 seconds. |  Cervical FPR |
| Thoracic Spine FPR: The patient is seated. The physician's hand opposite the side of the prominent transverse process monitors the dysfunction. The other hand is placed across the shoulder girdle overlying the trapezius. The patient is taken into the dysfunctional position and the patient is asked to sit straight up until the thoracic curve is flattened. A gentle axial compression is applied down the axial spinefor 3 to 5 seconds. (Note: Alternatively, the physician may place their hand posterior or anterior to the patient's head.) | 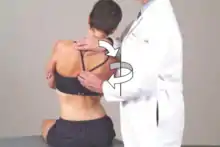 Thoracic FPR |
| Lumbar Type 1 Dysfunction FPR: The patient lies prone. The physician stands on the side opposite the prominent lumbar transverse process and monitors the dysfunctional segment. The physician rests their knee on the patient's ilium and crosses the ankle on the dysfunctional side over the other ankle while sliding the patient's legs to the side opposite the prominent transverse process. The physician grasps the patient's thigh and directs a force dorsally and toward external rotation to apply a gentle axial compressive force for 3 to 5 seconds. (Note: The legs should be moved toward the non-dysfunctional side in order to induce sidebending; axial compression is the last step.) |  Lumbar Type 1 FPR |
| Lumbar Type 2 Dysfunction FPR: The patient lies in the lateral recumbent position opposite the side of the prominent lumbar transverse process. The physician stands in front of the patient. The physician's forearm and hand control the right anterolateral chest wall and the other forearm and hand control the pelvic and lumbar regions. The physician monitors the transverse process of the dysfunctinal segment. The hips are flexed to the level of the dysfunction. The physician brings the forearms together to apply a gentle axial compression for 3 to 5 seconds. (Note: The dysfunctional rotation side should be facing upward.) |  Lumbar Type 2 FPR |
Still techniques
Still techniques are performed by moving the dysfunctional segment into its ease of motion, followed by the addition of an appropriate amount of compression. While maintaining compression, with moderate acceleration, move the segment toward the restrictive barrier. The compression is slowly released before the restrictive barrier is fully engaged, and the patient is returned to neutral.
| Elevated Acromioclavicular (AC) joint: The patient is seated. The physician stands behind the patient toward the dysfunctional side. The physician, using the hand closest to the patient, places the second metacarpal-phalangeal joint over the distal third of the clavicle to be treated. The physician maintains constant caudad pressure over the patient’s clavicle throughout the treatment sequence. The physician’s other hand grasps the patient’s arm on the side to be treated just below the elbow. The patient’s arm is pulled down and then drawn backward into extension with a continuous motion similar to throwing a baseball, circumducting the arm until it is once again in front of the patient, finishing with the arm across the chest in adduction.
|
 Elevated AC Still Technique |
| Elevated Sternoclavicular (SC) joint: The patient is seated. The physician stands behind the patient with the left hand reaching around in front of the patient. The physician's thumb is placed over the proximal end of the patient's right clavicle. The thumb maintains constant downward pressure. The other hand grasps just below the elbow on the side of the dysfunctional clavicle and the arm is brought toward flexion from adduction to abduction. With a continuous backstroke motion, similar to throwing a softball, the arm is circumducted toward extension until it is at the side of the patient. At this point, the arm is brought forward and placed across the chest.
|
 Elevated SC Still Technique |
| Elevated Rib 1: The patient is seated. The physician stands behind the patient. The physician's hand on the non-dysfunctional side reaches over the patient's non-dyfsunctional shoulder and across the patient's chest to lie palm down over the patient's dysfunctional shoulder with the second and third finger pads anchoring the first rib. The physician's hand on the dysfunctional side bends the patient head to the non-dysfunctional side while the other arm keeps the trunk stable. The physician's hand on the dysfunctional side adds a gentle compression force toward the dysfunctional first rib. The patient is instructed to inhale and exhale. On exhalation, the physician pushes the patient's head to the dysfunctional side maintaining compression on the rib. The patient is taken toward the restrictive barrier.
|
 Elevated Rib 1 Still Technique |
| Depressed Rib 1: The patient is seated. The physician stands behind the patient. The physician's hand on the side of the dysfunctional rib palpates the posterior aspect of the first rib at the costotransverse articulation attachment. The opposite hand is placed over the patient's head. The physician's hand on the non-dysfunctional side slowly flexes the patient's head until T1 and the first rib are engaged. The head and sidebent and rotated toward the side of the dysfunctional rib. The patient is instructed to exhale. On inhalation, the head is taken toward the opposide side of sidebending and rotation. As the dysfunctional rib is engaged, a slight extension of the head is idnuced and this motion is carried toward the inhalation restrictive barrier.
|
 Depressed Rib 1 Still Technique |
Review Questions
1. A 37-year-old female presents complaining of tenderness along the left proximal lateral lower leg. Past medical history is notable for hypertension for which she takes amlodipine 5 mg 1 tab daily. Vital signs show blood pressure of 130/86, heart rate 74, and temperature 98.4 F. Physical exam is unremarkable for heart and lungs. Focused musculoskeletal exam shows unremarkable provocative testing of the left knee. While assessing ankle motion, she shows preference for inversion of the ankle and restriction with eversion of the ankle. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of the bilateral lower extremities is unremarkable. Which of the following correctly describes the disengagement and ease setups, respectively, for BLT treatment for the osteopathic exam findings noted?
A. Push the left distal tibia into the table; push the distal left tibia posteriorly
B. Push the left fibula caudad along the length of the fibula with the dominant hand proximally and the non-dominant hand distally; invert and internally rotate the left foot
C. Apply compression or traction to the knee; externally rotate the tibia
D. Distract the calcaneus from the talus; plantarflex the forefoot
2. A 40-year-old male presents complaining of right ankle pain. Past medical history is unremarkable. Vital signs show blood pressure of 120/84, heart rate 72, and temperature 97.6 F. Physical exam is unremarkable for heart and lungs. While assessing foot motion, he shows restriction of translation of anterior translation of the right tibia and fibula on the right talus. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of the bilateral lower extremities is unremarkable. Which of the following correctly describes the disengagement and ease setups, respectively, for BLT treatment for the osteopathic exam findings noted?
A. Push the left distal tibia into the table; push the distal left tibia posteriorly
B. Push the left fibula caudad along the length of the fibula with the dominant hand proximally and the non-dominant hand distally; invert and internally rotate the left foot
C. Apply compression or traction to the knee; externally rotate the tibia
D. Distract the calcaneus from the talus; plantarflex the forefoot
3. A 34-year-old male presents to his primary care physician complaining of right-sided neck pain. Past medical history is unremarkable. Vital signs show blood pressure of 126/86, heart rate 82, and temperature 97.8 F. Physical exam is unremarkable for heart and lungs. Cervical spine range of motion testing shows restriction in extension. Segmental motion testing reveals restriction and a prominence on the right side overlying the articular pillar at the level of C4. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of the bilateral upper extremities is unremarkable. What is the appropriate initial setup for facilitated positional release of this somatic dysfunction?
A. With the right hand on the supine patient's head, the cervical spine is neutralized by a slight flexion followed by application of an activating force in the form of a gentle axial compression while the patient's head is positioned toward flexion, right sidebending, and right rotation for 3 to 5 seconds.
B. With the left hand on the supine patient's head, the cervical spine is neutralized by a slight flexion followed by application of an activating force in the form of a gentle axial compression while the patient's head is positioned toward flexion, left sidebending, and left rotation for 3 to 5 seconds.
C. With the right hand on the supine patient's head, the cervical spine is neutralized by a slight flexion followed by application of an activating force in the form of a gentle axial compression while the patient's head is positioned toward flexion, left sidebending, and left rotation for 3 to 5 seconds.
D. With the left hand on the supine patient's head, the cervical spine is neutralized by a slight flexion followed by application of an activating force in the form of a gentle axial compression while the patient's head is positioned toward flexion, right sidebending, and right rotation for 3 to 5 seconds.
4. A 26-year-old female presents to her primary care physician complaining of mid-back pain. Past medical history is unremarkable. Vital signs show blood pressure of 136/76, heart rate 78, and temperature 97.4 F. Physical exam is unremarkable for heart and lungs. Thoracic spine range of motion testing shows restriction in flexion. Segmental motion testing reveals restriction and a prominence on the right side overlying the transverse process of T6. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of is unremarkable. What is the appropriate initial setup for facilitated positional release of this somatic dysfunction?
A. the patient's thoracic curve is flattened in extension is palpated at the spinous process of T7, compression is applied as the patient is taken further into extension, right sidebending, and right rotation for 3-5 seconds
B. the patient's thoracic curve is flattened in extension is palpated at the spinous process of T6, compression is applied as the patient is taken further into extension, right sidebending, and right rotation for 3-5 seconds
C. the patient's thoracic curve is flattened in extension is palpated at the spinous process of T6, compression is applied as the patient is taken further into flexion, right sidebending, and right rotation for 3-5 seconds
D. the patient's thoracic curve is flattened in extension is palpated at the spinous process of T7, compression is applied as the patient is taken further into flexion, left sidebending, and left rotation for 3-5 seconds
5. A 45-year-old female presents to her primary care physician complaining of low back pain. Past medical history is unremarkable. Vital signs show blood pressure of 126/86, heart rate 88, and temperature 98.4 F. Physical exam is unremarkable for heart and lungs. Range of motion testing of the lumbar spine shows no restriction in either flexion or extension. Segmental motion testing reveals restriction and a prominence on the right side overlying the transverse process of L3. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of is unremarkable. What is the appropriate initial setup for facilitated positional release of this somatic dysfunction with the patient in a supine position?
A. the physician's right hand raises the patient's right leg and externally rotates it; the physician's left hand applies a compressive force over the right L4 transverse process
B. the physician's left hand raises the patient's left leg and externally rotates it; the physician's right hand applies a compressive force over the left L4 transverse process
C. the physician's left hand raises the patient's right leg and externally rotates it; the physician's right hand applies a compressive force over the left L4 transverse process
D. the physician's right hand raises the patient's left leg and externally rotates it; the physician's left hand applies a compressive force over the right L4 transverse process
6. A 38-year-old male presents to her primary care physician complaining of low back pain. Past medical history is unremarkable. Vital signs show blood pressure of 136/82, heart rate 68, and temperature 97.8 F. Physical exam is unremarkable for heart and lungs. Range of motion testing of the lumbar spine shows restriction in extension. Segmental motion testing reveals restriction and a prominence on the right side overlying the transverse process of L4. Neurologic exam of deep tendon reflexes, muscle strength, and sensation of is unremarkable. What is the appropriate initial setup for facilitated positional release of this somatic dysfunction with the patient in a left lateral recumbent position?
A. the patient's shoulder is rotated anteriorly and the patient's hips, flexed to the level of L4, are rotated anteriorly as a compressive force is applied for 3 to 5 seconds
B. the patient's shoulder is rotated posteriorly and the patient's hips, flexed to the level of L4, are rotated posteriorly as a compressive force is applied for 3 to 5 seconds
C. the patient's shoulder is rotated anteriorly and the patient's hips, flexed to the level of L4, are rotated posteriorly as a compressive force is applied for 3 to 5 seconds
D. the patient's shoulder is rotated posteriorly and the patient's hips, flexed to the level of L4, are rotated anteriorly as a compressive force is applied for 3 to 5 seconds
7. A 20-year-old male presents to his primary care physician complaining of worsening asthma exacerbations despite albuterol inhaler use. Vital signs show blood pressure of 130/80, heart rate 74, and temperature 98.2 F. Physical exam is unremarkable for heart and lungs. Range of motion testing of the ribs show a restriction of motion of the right first rib with exhalation. What is the appropriate treatment setup for this somatic dysfunction using a Still technique?
A. the patient’s head is sidebent to the left as the physician’s right hand applies a compressive force with the force vector directed toward the first rib while the patient breathes followed by the patient's head being sidebent to the right and the compressive force maintained on the rib toward the restrictive barrier
B. the patient's head is sidebent and rotated to the right and the patient breathes followed by the the head being carried to a position of right sidebending and rotation with a slight extension and pump handle motion occuring as the restrictive barrier is engaged
C. the patient’s affected arm on the side of the dysfunction and pulls down, drawing the clavicle into extension taking the arm through circumduction until it is again in front of the patient and ending with the arm across the chest in adduction
D. a constant inferior pressure is applied and maintained on the dysfunctional side as the patient’s arm is brought just below and the arm through flexion from adduction to abduction until it is again brought into extension
8. A 68-year-old female presents to his primary care physician complaining of cough despite compliance with his COPD medications. Vital signs show blood pressure of 120/86, heart rate 72, and temperature 97.6 F. Physical exam is unremarkable for heart and lungs show decreased breath sounds at the bilateral lung bases. Range of motion testing of the ribs show a restriction of motion of the right first rib with inhalation. What is the appropriate treatment setup for this somatic dysfunction using a Still technique?
A. the patient’s head is sidebent to the left as the physician’s right hand applies a compressive force with the force vector directed toward the first rib while the patient breathes followed by the patient's head being sidebent to the right and the compressive force maintained on the rib toward the restrictive barrier
B. the patient's head is sidebent and rotated to the right and the patient breathes followed by the the head being carried to a position of right sidebending and rotation with a slight extension and pump handle motion occurring as the restrictive barrier is engaged
C. the patient’s affected arm on the side of the dysfunction and pulls down, drawing the clavicle into extension taking the arm through circumduction until it is again in front of the patient and ending with the arm across the chest in adduction
D. a constant inferior pressure is applied and maintained on the dysfunctional side as the patient’s arm is brought just below and the arm through flexion from adduction to abduction until it is again brought into extension
9. A 23-year-old male professional athlete presents to his primary care physician's office complaining of pain overlaying his anterior right shoulder. Past medical history is unremarkable. Vital signs show blood pressure of 124/82, heart rate 70, and temperature 98.2 F. Range of motion testing reveals a sternoclavicular joint that glides inferiorly on the left with shoulder shrug and has no appreciable motion on the right. What is the appropriate treatment setup for this somatic dysfunction using a Still technique?
A. the patient’s head is sidebent to the left as the physician’s right hand applies a compressive force with the force vector directed toward the first rib while the patient breathes followed by the patient's head being sidebent to the right and the compressive force maintained on the rib toward the restrictive barrier
B. the patient's head is sidebent and rotated to the right and the patient breathes followed by the the head being carried to a position of right sidebending and rotation with a slight extension and pump handle motion occuring as the restrictive barrier is engaged
C. the patient’s affected arm on the side of the dysfunction and pulls down, drawing the clavicle into extension taking the arm through circumduction until it is again in front of the patient and ending with the arm across the chest in adduction
D. a constant inferior pressure is applied and maintained on the dysfunctional side as the patient’s arm is brought just below and the arm through flexion from adduction to abduction until it is again brought into extension
10. A 32-year-old femmale professional dancer presents to her primary care physician's office complaining of pain overlaying her anterior right shoulder. Past medical history is unremarkable. Vital signs show blood pressure of 120/80, heart rate 73, and temperature 98.4 F. Range of motion testing reveals demonstrate the left proximal clavicle is more caudad and posterior. What is the appropriate treatment setup for this somatic dysfunction using a Still technique?
A. the patient’s head is sidebent to the left as the physician’s right hand applies a compressive force with the force vector directed toward the first rib while the patient breathes followed by the patient's head being sidebent to the right and the compressive force maintained on the rib toward the restrictive barrier
B. the patient's head is sidebent and rotated to the right and the patient breathes followed by the the head being carried to a position of right sidebending and rotation with a slight extension and pump handle motion occuring as the restrictive barrier is engaged
C. the patient’s affected arm on the side of the dysfunction and pulls down, drawing the clavicle into extension taking the arm through circumduction until it is again in front of the patient and ending with the arm across the chest in adduction
D. a constant inferior pressure is applied and maintained on the dysfunctional side as the patient’s arm is brought just below and the arm through flexion from adduction to abduction until it is again brought into extension
Answers to Review Questions
- B
- A
- D
- B
- A
- D
- A
- B
- C
- D