Chapter 4: Thoracic Spine
Objectives:
- Describe the anatomy and musculature of the thoracic spine
- Describe and apply the rule of threes
- Describe the major motions of the thoracic spine: rotation, sidebending, flexion, and extension
- Describe Fryette’s Laws of Physiologic Motion
- Identify the primary muscles that cause rotation, sidebending, flexion, and extension of the thoracic spine and their attachments and innervation
- Identify the components of the vertebra of the thoracic spine: transverse process, spinous process, lamina, pedicle, body, transverse foramen, posterior tubercle, anterior tubercle, superior articular process, inferior articular process, costal facet of transverse process, superior vertebral notch, and inferior vertebral notch
- Identify the anterior and posterior counterstrain points: Anterior: 1-6 midline, 7-12 bilateral; Posterior: 1-12 spinous/transverse processes
Anatomy and Musculature of the Thoracic Spine
The thoracic cage includes 12 thoracic vertebrae, 12 pairs of ribs, and the sternum. The thoracic vertebrae can be broken up into three regions: the upper (T1-T4), middle (T5-T8), and lower (T9-T12/L1). Three main functions of the thoracic spine are to protect the spinal cord, to allow movement of the torso, and to support the upper body. The upper vertebrae are smaller than the lower vertebrae because the lower vertebrae have to bear more weight. (This size will be seen to be even larger in the lumbar spine.) The thoracic spine has a gentle kyphosis and serves as a transition zone between the cervical and lumbar spines. T1-T2 show the transition of the cervical lordosis. T3-T12 demonstrate the thoracic kyphosis characteristic of the thoracic spine. The apex of the thoracic kyphosis is at T5-T6. At the level of T10-T12 the transition to lumbar lordosis becomes apparent.
The functional landmarks used in palpating and diagnosing the thoracic spine include:
- The suprasternal notch, which is anterior the vertebral body of T2.
- The spine of the scapula corresponds to the spinous process of T3.
- The angle of Louis (the sternal angle) corresponds anteriorly to T4.
- The xiphoid process is anterior to T9.
- The inferior angle of the scapula corresponds to the spinous process of T9.
The vertebrae of the thoracic spine, like the cervical spine, are characterized as typical versus atypical vertebrae. The vertebral arch is made of the lamina and the pedicle. The lamina is a posterior arch that lies between the spinous and transverse processes. The pedicle connects the body of a vertebrae to its corresponding transverse process. Typical thoracic vertebrae have a heart-shaped body and possess two demifacets which articulate with the heads of the ribs. The spinous processes, a posterior projection of a vertebrae where the lamina of the vertebral arch join as well as serving as attachments of muscles and ligaments, are long and slope downward. The vertebral arches are made of the lamina and the pedicle. The lamina connects the spinous process to the transverse processes. The transverse processes are bony projection bilaterally located which serve as attachment sites of muscles and ligaments. On the transverse process is the costal facet for the attachment of the rib, and it is the transverse process itself which is used to diagnose somatic dysfunctions. The pedicles connect the posterior portion of the vertebrae to the anterior portion. Facet joints are located between the articular processes of two adjacent vertebrae and determines physiologic motion. The motion of the superior facet joints of the thoracic spine is backward, upward, and lateral; the motion of the interior facet joints is forward, downward, and medial. Atypical thoracic vertebrae include T1, T9, T11, and T12. T1 is strikingly similar to the lower cervical vertebrae. T9 has no inferior demifacet. T11 and T12 have a single costal facet that articulates with the atypical ribs 11 and 12 respectively; additionally, there are no facets on the transverse processes of T11 or T12. Physiologic motion of the thoracic spine is determined by the orientation of the facet joints. Other significant anatomic landmarks of the thoracic spine include the body, the transverse foramen, the posterior tubercle, the anterior tubercle, the superior articular process, the inferior articular process, the superior vertebral notch, and the inferior vertebral notch.
The rule of threes describes the relative position of the spinous processes to the transverse processes of vertebrae in the thoracic spine:
- T1-T3, T12: spinous process is located at the level of corresponding transverse process
- T4-T6, T11: spinous process is located ½ segment below corresponding transverse process
- T7-T9, T10: spinous process is located at the level of the transverse process one vertebrae below
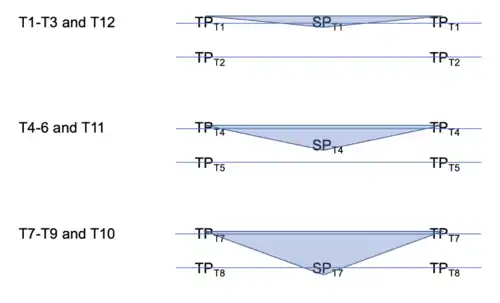 Rule of threes |
| Example: Applying the rule of threes |
|---|
| The spinous process of T9 is located at the level of the transverse process of T10. |
Biomechanically, thoracic spine motion is smaller compared to that of the cervical and lumbar spines because the ribs hinder this motion. The upper and middle thoracic spine have greater rotation and flexion. The lower thoracic spine has greater sidebending and even better flexion and extension. (For example – sidebending range of motion: T1-T4: 5-25o; T5-T8: 10-30o; T9-T12: 30-45o; rotation range: T9-T12: 30-45o) Thus, the primary motion of the thoracic spine is rotation, followed by sidebending, then flexion, then extension. Why is thoracic motion limited? Ribs 2-10 prevent rotation. The sternal rib attachments and posterior ligaments prevent flexion. The anterior longitudinal ligaments, facets, lamina, and spinous processes prevent extension. Most free movement occurs at the level of T11-T12 where the floating ribs are attached.
Superficial muscles of the thoracic and lumbar spine include the levator scapulae, rhomboid minor, rhomboid major, deltoid, teres major, latissimus dorsi, trapezius, and serratus posterior inferior muscles. (Table 4.1)
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Levator scapulae | C1-C4 transverse processes | Superior angle of the scapula | Medial and upward movement of scapula | Dorsal scapular nerve (C4-C5) | 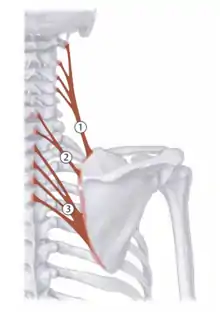 1 - levator scapulae |
| Rhomboid minor | C6-C7 spinous processes | Medial border of scapula | Medial and upward movement of scapula | Dorsal scapular nerve (C4-C5) | 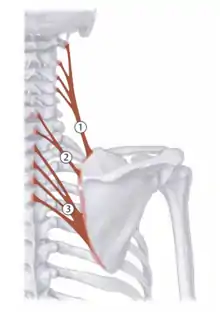 2 - rhomboid minor |
| Rhomboid major | T1-T4 spinous vertebrae | Medial border of scapula | Medial and upward movement of scapula | Dorsal scapular nerve (C4-C5) | 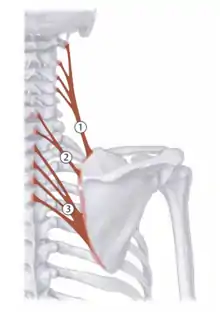 3 - rhomboid major |
| Deltoid |
|
Deltoid tuberosity on humerus |
|
Axillary nerve (C5-C6) | 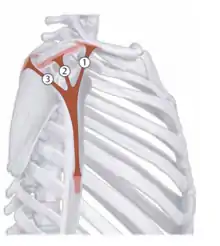 Deltoid: 1 - anterior; 2 - medial; 3 - posterior |
| Teres major | Inferior angle of scapula | Lesser tuberosity of humerus | Internal rotation, adduction | Subscapular nerve (C5-C6) | 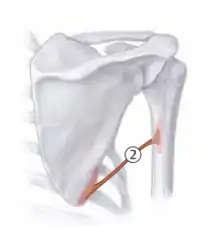 2 - teres major |
| Latissimus dorsi | T7-T12 spinous processes; iliac crest; ribs 9-12 | Lesser tuberosity of the humerus | Internal rotation, adduction, retroversion; respiration (“cough” muscle) | Thoracodorsal nerve (C6-C8) | 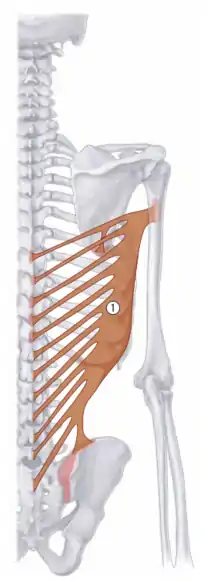 1 - latissimus dorsi |
| Trapezius muscle |
|
|
|
CN XI, cervical plexus (C2-C4) | 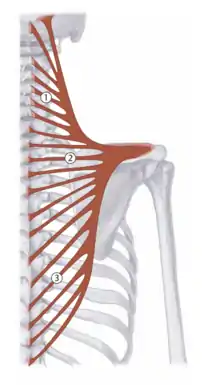 Trapezius: 1 - descending; 2 - transverse; 3 - ascending |
| Serratus posterior superior | Nuchal ligament, SPs of C7-T3 | Ribs 2-5 | Elevate ribs 2-5; respiration | 2nd through 5th intercostal nerves | No schematic |
| Serratus posterior inferior | Spinous processes of T11-L2 | Ribs 9-12 | Depress ribs 9-12; respiration | 9th through 12th intercostal nerves | No schematic |
Intermediate muscles of the back include the longissimus thoracis, spinalis thoracis, iliocostalis thoracis, iliocostalis lumborum, and semispinalis thoracis muscles. The erector spinae muscles include the iliocostalis, the longissimus, and the spinalis muscles; these muscles extend and sidebend the vertebral column, allow flexion by decreasing resistance, and are vulnerable to trauma often leading to non-neutral (type 2) dysfunctions.
The deep back muscles include the rotatores and multifidus; these muscles participate in proprioception, maintenance of posture and directing movement, are vulnerable to trauma, maintain non-neural dysfunctions, and are often involved in viscerosomatic reflexes. The rotatores brevis and rotatores longus as well as the intertransversarii, interspinalis, and short rotator muscles are intricately attached from one spinal level to the next.
Connective tissue and fascia surround all organs, muscles, and vessels. Endothoracic fascia blends with ribs and the sternum as well as covers the superior surface of the diaphragm. It is continuous with cervical fascia and attaches to the first rib as well as the pericardium, the pleura, and the mediastinum. An increase in the fascial sheet tension in one area alters angles of fascial bands and changes cross-linkages between the bands. This results in altered lymph flow, blood flow, neural innervation, muscle function, and organ function. Normalization of fascial tensions returns the body to more efficient function.
The thoracic vertebrae contain the intervertebral discs which contain the anulus fibrosis and nucleus pulposus. The nucleus pulposus is the inner core of the vertebral disc that withstands forces of compression and torsion. The anterior longitudinal ligament is responsible for limiting spinal extension by strongly attaching at the vertebral bodies. The posterior longitudinal ligament is attached posteriorly to the vertebral bodies and forms the anterior wall of the spinal canal. The intertransverse ligaments limit sidebending of the vertebrae and attach one transverse process to the next. The ligamenta flava attach one vertebral arch to the next.
Thoracic spine motion is less than cervical and lumbar; ribs hinder its motion. The upper and middle thoracic spine have greater rotation and flexion. Lower thoracic spine has greater sidebending and even better flexion and extension due to the presence of the floating ribs. Ribs 2-10 prevent rotation. The sternal rib attachments and posterior ligaments prevent forward bending. The anterior longitudinal ligament, facets, lamina, and spinous processes prevent backward pending. The freest area of motion is T11-T12 range where the floating ribs are attached as well as the spinous process having a more horizontal structure.
Forward-bending of the thoracic spine (i.e. flexion) involves approximation or compression of the anterior vertebral parts and a distraction or separation of the posterior vertebral parts; these motions occur about a transverse axis. Backward-bending (i.e. extension) involves approximation of the posterior vertebral parts and distraction of the anterior vertebral parts; these motions occur about a transverse axis just like forward bending. Excessive flexion can lead to disc herniations. Rotation involves turning of the vertebral segment around a longitudinal axis.
Somatic Dysfunctions of the Thoracic Spine
Fryette’s Laws of Physiologic Motion dictate biomechanics of somatic dysfunction of the thoracic and lumbar spine:
- Fryette’s First Law states when the thoracic and lumbar spine are in a neutral position, the coupled motion of sidebending and rotation for a group of vertebrae occur to opposite sides.
- Fryette’s Second Law states when the thoracic and lumbar spine is sufficiently flexed or extended (non-neutral), the coupled motions of sidebending and rotation in a single vertebra occur to the same side; the facet joints are engaged and dictate which direction the body of the vertebrae moves.
- Fryette’s Third Law states initiating motion of a vertebral segment in any plane of motion will modify the movement of that segment in other planes of motion
| Example: Somatic dysfunction nomenclature |
|---|
Type 1 dysfunction:
(in type 1 dysfunctions, sidebending is written first) |
Type 2 dysfunction:
(in type 2 dysfunctions, rotation is written first) |
With right sidebending, the right transverse process moves inferiorly, the left transverse process moves superiorly, and a concavity is noted on the sidebent side. (Likewise, convexity is noted on the contralateral side.)
| Example: Diagnosing thoracic spine somatic dysfunctions |
|---|
| Upon palpation of a patient’s thoracic spine, T7 is found to have a prominent transverse process on the right. The T7 location is verified by locating the inferior angle of the scapula. The transverse processes of the vertebrae above and below this level are unremarkable. With extension, the prominence of the transverse process of T7 is not appreciated. With flexion, the prominence is more apparent. The somatic dysfunction diagnosis is T7 ERRSR. |
Treatment of Somatic Dysfunction of the Thoracic Spine
Physicians should use the regional motion findings and then compare segmental motion of each affected level in order to make an appropriate diagnosis. Muscle hypertonicity will be apparent as will prominence of transverse processes. In terms of treating somatic dysfunctions, the same principles as with the cervical spine apply. Myofascial release/Soft tissue techniques should be performed first and certainly prior to performing any muscle energy or HVLA techniques. Counterstrain techniques should be done similarly to those of the cervical spine utilizing the corresponding tenderpoint. Please review Chapter 2 for mechanisms, relative contraindications, and absolute contraindications to these techniques.
Some examples of myofascial release techniques include:
| Thoracodorsal fascia: The patient is prone. Place both hands on opposite sides of the thoracodorsal fascia. Apply enough pressure to engage the fascial tissue until suf- ficient end feel is reached. Assess motion of the tissue in all 3 planes of motion: anterior/posterior (representing flexion and extension), clockwise and counterclockwise twisting (representing rotational component), and tilting from one hand to the other (representing the sidebending component). Ease of motion in all planes is determined. This technique can then be used as either a direct or an indirect technique. If performing a direct technique, bring the fascia into patient’s barrier in all three planes of motion. If performing an indirect technique, bring the fascia in all three planes into its ease of motion. Hold the tissues in either the ease or barrier of motion in all three planes. This force is held for approximately 30-60 seconds or until a release is palpated. |  Thoracodorsal fascia |
| Unilateral prone pressure: The patient is prone with the physician on the opposite side of the region to be treated. The physician places their thumb and thenar eminence of one hand on the paraspinal thoracic musculature above the transverse processes and placed the other hand on top of the abducted thumb on the bottom hand over the other hand. The elbows are kept straight and a downward force is applied followed by a lateral, perpendicular stretch for 3-5 seconds. The force is released and the process is repeated for a total of 30 seconds. Reassessment of the thoracic spine can be done by assessing active and passive ranges of motion compared to those prior to performing the technique and also by reassessing tissue texture changes/TART. |  Unilateral prone pressure |
| The "alternating catwalk" variation of unilateral prone pressure: The patient is prone with the physician on the opposite side of the region to be treated. The physician places their hands on the medial aspect of the thoracic paraspinal muscles above the transverse processes and adds a downward lateral force with the caudad hand which is held for 3-5 seconds. As the force is released with the caudad hand, the cephalad hand begins to add a downward lateral force. The process is repeated for 30 seconds. Reassessment of the thoracic spine can be done by assessing active and passive ranges of motion compared to those prior to performing the technique and also by reassessing tissue texture changes/TART. | |
| Bilateral prone pressure/counterpressure: The patient is prone with the physician on the opposite side of the region to be treated. The physician places the thumb and thenar eminence of the caudad hand on the medial aspect of the thoracic paraspinal muscles over the transverse processes on the opposite side with the fingers pointing cephalad. The physician places the hypothenar eminence of the cephalad hand on the medial aspect of the patient's paraspinal musculature ipsilateral to the side on which the physician is standing with the fingers pointing caudad. A separating and distraction force is applied and held for 3-5 seconds and repeated in a rhythmic fashion for 30 seconds. Reassessment of the thoracic spine can be done by assessing active and passive ranges of motion compared to those prior to performing the technique and also by reassessing tissue texture changes/TART. |  Bilateral prone pressure |
| Bilateral thumb pressure: The patient is prone with the physician's thumbs bilaterally contacting the paraspinal muscles over the transverse processes of T1 and apply a gentle anterior and inferolateral force for 3-5 seconds and repeated in a rhythmic fashion. The thumbs are placed over the successive transverse processes of the remaining levels of the thoracic spine until T12 is reached. The physician them moves to the pelvis and, starting at the transverse process of T12, applies an anterior and superolateral force along the successive levels of the thoracic spine and also by reassessing tissue texture changes/TART. |  Bilateral thumb pressure |
Some examples of myofascial release techniques include:
| T1-T4 (head assist): | |
|---|---|
| Type 1 somatic dysfunctions: The patient is seated on the table, while the physician stands behind the patient. One hand monitors the transverse process of the vertebrae at the apex of the curve on the rotational side (left side if the group is rotated to the left, right side if the group is rotated to the right). The other hand is either placed on the patient’s head or wrapped around it for better control. The patient’s thoracic spine is kept in the neutral position, and then using the head, the spine is sidebent and rotated into its barriers of motion (sidebending occurs toward the convexity and rotation occurs away from the convexity). The patients is then instructed to sidebend and rotate their head toward their ease of motion (toward the diagnosis) and this force is met by the physician to produce an isometric contraction. The isometric contraction occurs for 3-5 seconds, and is repeated 3-5 cycles, resetting the thoracic spine to the new restrictive barrier after each successive contraction. Perform a final stretch after the final isometric contraction. | 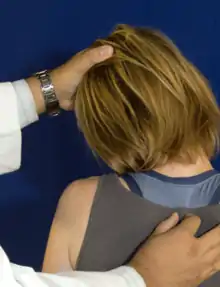 T1-T4 seated muscle energy for Type 1 and Type 2 dysfunctions |
| Type 2 somatic dysfunctions: The patient is seated on the table, while the physician stands behind the patient. One hand monitors the transverse process of the vertebrae on the rotation side of the dysfunction (right transverse process if the vertebra is rotated to the right). The other hand is either placed on the patient’s head or wrapped around it for better control. The patient’s thoracic spine is then flexed or extended into the barrier of motion, then using the head, the spine is side- bent and rotated into its barriers of motion. The patient is then instructed to sidebend or rotate their head toward their ease of motion (toward the diagnosis) and this force is met by the physician to produce an isomet- ric contraction. The isometric contraction occurs for 3-5 seconds, and is repeated 3-5 cycles, resetting the thoracic spine to the new restrictive barrier after each successive contraction. Perform a final stretch after the final isometric contraction. | 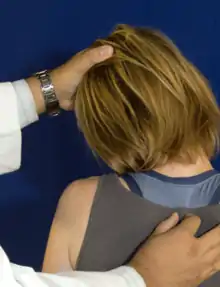 T1-T4 seated muscle energy for Type 1 and Type 2 dysfunctions |
| T5-T12 (body assist) | |
| Type 1 somatic dysfunctions: The patient is seated on the table, while the physician stands behind the patient. One hand monitors the transverse process of the vertebrae at the apex of the curve on the rotational side (left side if the group is rotated to the left, right side if the group is rotated to the right). The other hand is placed across the patient’s shoulders, it may be helpful to have the patient hold their elbows in a genie position. The patient’s thoracic spine is kept in the neutral position, then using the shoulders for control, the spine is sidebent and rotated into its barriers of motion (sidebending occurs toward the convexity and rotation occurs away from the convexity). The patient is then instructed to sidebend and rotate their body toward their ease of motion (toward the diagnosis) and this force is met by the physician to produce an isometric contraction. The isometric contraction occurs for 3-5 seconds, and is repeated 3-5 cycles, resetting the thoracic spine to the new restrictive barrier after each successive contraction. Perform a final stretch after the final isometric contraction. | 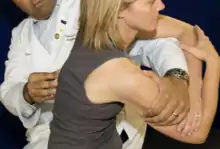 T5-T12 seated muscle energy for Type 1 dysfunctions |
| Type 2 somatic dysfunctions: The patient is seated on the table, while the physician stands behind the patient. One hand monitors the transverse process of the vertebrae on the rotation side of the dysfunction (right transverse process if the vertebra is rotated to the right, left transverse process if the vertebra is rotated to the left). The other hand is placed across the patient’s shoulders, it may be helpful to have the patient hold their elbows in a genie type position. The patient’s thoracic spine is then flexed or extended into the barrier of motion, then using the body, the spine is sidebent and rotated into its barriers of motion. The patient is then instructed to sidebend or rotate their body toward their ease of motion (toward the diagnosis) and this force is met by the physician to produce an isometric contraction. The isometric contraction occurs for 3-5 seconds, and is repeated 3-5 cycles, resetting the thoracic spine to the new restrictive barrier after each successive contraction. Perform a final stretch after the final isometric contraction. |  T5-T12 seated muscle energy for Type 2 dysfunctions |
Myofascial release should be performed prior to performing HVLA. This relaxes muscles, stretches connective tissue, and instills confidence in the patient. The physician can also take advantage of respiratory effort to assist. Barriers in all planes of motion (flexion/extension, sidebending, and rotation) should be engaged. It is important to recognize guarding – do not thrust if the patient is apprehensive, if the patient is tensing muscles, if the patient stops breathing through the respiratory cycle, or if the patient reports pain. When treating a region with an HVLA technique, the vertebral segment in the middle of the dysfunction is where the thrust should be targeted.
Some examples of HVLA techniques include:
| Seated HVLA (Full Nelson): The patient is seated on the table, while the physician stands behind the patient. The patient is instructed to interlock their hands behind her head. The physician weaves their arms from anterior to posterior through the opening created by the patient’s arms, and interlocks their hands on top of the patient’s hands. The patient is instructed to bring their elbows together and relax and look up toward the ceiling. The physician then brings the dysfunctional transverse process or apex of a group dysfunction into contact with the physician’s sternum. The physician instructs the patient to take a deep breath in and out. At the end of exhalation with the physician’s knees bent, the physician exerts a quick but gentle thrust superiorly and posteriorly from their legs. |  Full Nelson |
| Supine HVLA (Kirskville Crunch): The patient is supine on the table with the physician standing on the side opposite the rotational component (on the left side of the patient if the dysfunction is rotated to the right and on the right side of the patient if the dysfunction is rotated to the left). The patient’s arms are crossed across the chest and the patient is instructed to grasp their shoulders. The arm of the dysfunctional side should be on top. The physician uses one arm on the patient’s elbows to roll the patient towards the physician, lifting the dysfunction-side shoulder blade off the table. The physician places the thenar eminence of the other hand over the posterior transverse process or at the apex of the curve for a group dysfunction. The patient’s elbows are placed in the physician’s abdomen just inferior to the xiphoid process. The physician takes the hand that was positioning the elbows and places it under the patients’ upper thoracic spine. The physician than adds slight sidebending into the barrier to further engage the restrictive barrier. The patient is instructed to inhale and then exhale. At the end exhalation, the physician exerts a rapid downward thrust through the patient’s arms into the transverse process resting on the physician’s thenar eminence. | 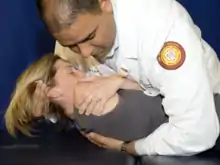 Kirksville Crunch |
| Prone HVLA (Texas Twist): The patient is prone on the table, while the physician stands on one side of the table. The physician places the thenar eminence of one hand over the transverse process of the posterior vertebrae or at the apex of the curve for a group dysfunction. The physician places the other hand over the opposite transverse process at one level below the rotational dysfunction. The physician then applies a downward (anterior) force and superior force with the one hand while also applying a downward (anterior) force and inferior force with the other hand. This motion is applied to take the dysfunction to its barrier in the sidebending plane of motion. The patient is instructed to inhale and then exhale. The physician locks the elbows and at the end of exhalation, applies a rapid, downward force thrust anteriorly with the hand on the posteriorly rotated dysfunction. |  Texas Twist |
Counterstrain shortens the strained muscle by bringing the origin and insertion closer. A tenderpoint is a small area of soft tissue which is tender to touch. Tenderpoints can be located anteriorly and posteriorly. Counterstrain techniques are indirect techniques where the patient is taken into the position of ease, with some exceptions.
To perform a counterstrain technique:
- A tenderpoint is identified by inquiring to the patient about tenderness.
- The physician labels the tenderpoint as a 10/10.
- The muscle is positioned such that the tenderpoint is no longer painful. The physician flexes, extends, sidebends, and rotates the involved muscle or joint to a point where there is a 70% reduction in pain rating (i.e. the patient states “the pain is now a 3/10”).
- The tenderpoint is monitored with one finger while the area remains in the position of comfort for 90 seconds.
- The muscle/joint is slowly and passively returned to neural while the tenderpoint is continually monitored.
- The degree of tenderness at the tenderpoint is reassessed.
| Thoracic counterstrain tenderpoints |
|---|
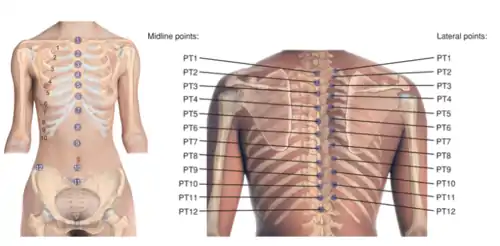 Thoracic Tenderpoints |
Reference: Nicholas AS, Nicholas EA. Atlas of Osteopathic Techniques. Philadelphia, PA: Lippincott Williams and Wilkins, 2016. Page 173.
| Tenderpoint | Location | Treatment position (initial setup) | Acronym |
|---|---|---|---|
| ATP1 | Midline episternal notch | Flex to dysfunctional level | F |
| ATP2 | Midline, junction of manubrium and sternum (angle of Louis) | Flexion to dysfunctional level | F |
| AT3-AT5 | Midline at level of corresponding rib | Flexion to dysfunctional level | F |
| AT6 | Midline xiphoid–sternal junction | Flexion to dysfunctional level | F |
| AT7–AT9 |
|
Flexion to dysfunctional level, side bending toward and rotation away | F STRA |
| AT10–AT12 |
|
Hip flexion 90–135 degrees, slight side bending, rotation toward (type I) or side bending toward, rotation away (type II) | F STRA |
| Tenderpoint | Location | Treatment position (initial setup) | Acronym |
|---|---|---|---|
| PT1–PT3 | Midline, or inferolateral tip of spinous process (side opposite rotational component) or over transverse process (on side of rotational component) | Prone with arms hanging over sides of table. Support patient's head by cupping point of chin; gently extend head and neck to engage dysfunctional segment. Avoid overextending. Rotation and sidebending minimal. |
|
| PT4–PT9 | Midline, or inferolateral tip of spinous process (side opposite rotational component) or over transverse process (on side of rotational component) | Prone with arms hanging over sides of table. Support patient's head by cupping point of chin; gently extend head and neck to engage dysfunctional segment. Avoid overextending. Rotation and sidebending minimal. Shoulders may be flexed fully to add extension or placed at the side to decrease extension with physician controlling shoulder from opposite side. |
|
| PT10–PT12 | Midline, or inferolateral tip of spinous process (side opposite rotational component) or over transverse process (on side of rotational component) | Patient prone with arms at side, physician controlling pelvis. |
|
Review Questions
1. Which of the following is paired correctly as an absolute or relative contraindication to thoracic muscle energy?
A. Fracture or dislocation is a relative contraindication.
B. Moderate to severe muscle strain is an absolute contraindication.
C. Moderate to severe joint instability is a relative contraindication.
D. Severe osteoporosis is an absolute contraindication.
E. Severe cardiopulmonary compromise is a relative contraindication.
2. Which of the following correctly describes the mechanism of action of the post-isometric muscle energy technique?
A. Post-isometric relaxation muscle energy is used to treat acute somatic dysfunctions.
B. Post-isometric relaxation muscle energy utilized the agonist/antagonist muscle of inverse relaxation with contraction placing the patient into their restriction to perform the technique.
C. Post-isometric relaxation muscle energy involves increasing pressure on Golgi tendon organ proprioceptors leading to reflex inhibition and subsequent muscle lengthening.
D. Post-isometric relaxation utilizes muscular attachments as fulcrums to mobilize joints with limited mobility.
E. Post-isometric relaxation utilizes respirations to move soma through a barrier.
3. A patient presents for evaluation of mid-back pain. On examination, she is found to have hypertonic paraspinal muscles at the levels of T5-T8. On segmental examination, T5-T8 are found to have restriction of motion with rotation to the left. Muscle strength testing, deep tendon reflexes, and sensation testing are unremarkable. What would be the initial setup prior to asking the patient to contract for muscle energy?
A. Thoracic spine neutral, sidebent left, rotated right
B. Thoracic spine extended, sidebent right, rotated left
C. Thoracic spine neutral, sidebent right, rotated left
D. Thoracic spine extended, sidebent right, rotated right
E. Thoracic spine flexed, sidebent left, rotated left
4. Extension of the thoracic spine is limited as a result of which ligament?
A. The anterior longitudinal ligament
B. The posterior longitudinal ligament
C. The intertransverse ligaments
D. The ligamenta flava
E. The interspinous ligament
5. A patient presents for evaluation of mid-back pain. On examination, she is found to have hypertonic paraspinal muscles at the levels of T3-T7. On segmental examination, T3-T7 are found to have restriction of motion with rotation to the left. Muscle strength testing, deep tendon reflexes, and sensation testing are unremarkable. What is the initial setup for a prone HVLA technique?
A. The physician stands on the right side of the table, the right hand is placed over the left half of the spine pointing caudad and the left hand is placed over the right half of the spine facing cephalad at the level of T3.
B. The physician stands on the right side of the table, the left hand is placed over the left hand of the spine pointing cephalad and the right hand is placed over the right half of the spine facing caudad at the level of T3.
C. The physician stands on the left side of the table, the left hand is placed over the left hand of the spine pointing caudad and the right hand is placed over the right half of the spine facing cephalad at the level of T3.
D. The physician stands on the left side of the table, the right hand is placed over the left hand of the spine pointing cephalad and the left hand is placed over the right half of the spine facing caudad at the level of T3.
6. The spinous process of T9 is located at the level of which transverse process?
A. T6
B. T7
C. T8
D. T9
E. T10
7. The transverse process of T10 is located at the level of which spinous process?
A. T8
B. T9
C. T10
D. T11
E. T12
8. What position should a patient found to have a T1 spinous process tenderpoint be placed?
A. Supine, with the thoracic spine flexed
B. Prone, with the thoracic spine extended
C. Lateral recumbent with the thoracic spine sidebent left
D. Lateral recumbent with the thoracic spine sidebent right
E. Prone with the thoracic spine sidebent right and rotated left
9. The anterior tenderpoints for T7-T9 are typically located ____; the anterior tenderpoints for T10-T11 are located ____.
A. at the xiphoid process; between umbilicus and pubic symphysis
B. on the sternum; between xiphoid process and umbilicus
C. in the intercostal space of respective ribs; just superior to ASIS
D. between xiphoid process and umbilicus; between umbilicus and pubic symphysis
E. on the sternum; just superior to ASIS
10. What is the orientation of the superior facet joints in the thoracic spine?
A. Backward, upward, medial
B. Backward, downward, medial
C. Backward, upward, lateral
D. Forward, downward, lateral
E. Forward, upward, medial
11. How is physiologic motion of the thoracic spine determined?
A. From tissue texture changes
B. From the presence of somatic dysfunction-associated restrictive barriers
C. From tenderness of the paraspinal muscles
D. From the orientation of the facet joints
E. From the flexibility and rigidity of the ribcage
12. A 25-year-old male presents for evaluation of common cold symptoms. Vital signs are stable and afebrile. On physical exam, he is noted to have a tenderpoint over the T1 spinous process. Paraspinal muscles at the spine of the scapula are found to be restricted in extension, rotation to the right, and sidebending to the right. Muscle strength, deep tendon reflexes, and sensation testing are unremarkable. What is the proper positioning for the initial setup of a counterstrain treatment technique?
A. E SARA
B. E SART
C. F SARA
D. F SART
E. E
13. Which of the following statements regarding Fryette’s Laws is correct?
A. Fryette’s Laws apply to the cervical, thoracic, lumbar, and sacral spines.
B. Fryette’s First Law states that group dysfunctions occur in flexion or extension.
C. Fryette’s Third Law states that motion in one plane has no effect on motion in other planes.
D. Fryette’s Second Law states that single vertebrae dysfunctions occur in flexion or extension in the thoracic and lumbar spine only.
E. Fryette’s Laws can be applied to the axial and appendicular skeleton.
14. Which of the following muscles comprise the erector spinae muscles?
A. Iliopsoas, latissimus dorsi, and semispinalis
B. Iliocostalis, longissimus, and spinalis
C. Rotatores, multifidus, and interspinalis
D. Iliocostalis, latissimus dorsi, and spinalis
E. Iliopsoas, longissimus, and semispinalis
15. Which longitudinal ligament of the thoracic spine is the most superficial?
A. Anterior longitudinal ligament
B. Ligamentum flavum
C. Supraspinous ligament
D. Posterior longitudinal ligament
16. Which of the following statements is true regarding the neuroanatomy of the thoracic spine?
A. There are 13 thoracic spinal nerve roots.
B. Each thoracic spinal nerve is named for the vertebra above it.
C. The dermatomes of the thoracic spine are located entirely on the trunk.
D. The thoracic spinal nerves are excluded from the paravertebral ganglia.
Questions 17-22: Match the following thoracic spine structure with the appropriate function.
17. Nucleus pulposus
18. Facet joint
19. Spinous process
20. Pedicle
21. Transverse process
22. Lamina
A. Connects the body of a vertebrae to its corresponding transverse process.
B. Inner core of the vertebral disc that withstands forces of compression and torsion.
C. Posterior projection of a vertebrae where the lamina of the vertebral arch join and serve as attachments of muscles and ligaments.
D. Located between the articular processes of two adjacent vertebrae.
E. Posterior arch that lies between the spinous and transverse processes.
F. Bony projection bilaterally located which serve as attachment sites of muscles and ligaments.
Answers to Review Questions
- E
- C
- A
- A
- B
- E
- B
- B
- D
- C
- D
- A
- D
- B
- C
- B
- B
- D
- C
- A
- F
- E