Chapter 12: Lymphatics
Objectives:
- Understand the role of the lymphatic system in regard to the circulatory system, filtration of fluids, inflammation, and the healing process.
- Understand the regional lymph drainage of lymph involving the right lymphatic duct and the thoracic (left lymphatic) duct.
- Understand the Sympathetic and parasympathetic autonomic systems and their effects on the lymphatic system.
- Understand the role of the various diaphragms and its importance in opening lymphatic pathways.
- Understand the importance of the technique order in treating the lymphatics.
- Understand the Relative and Absolute contraindications for lymphatic treatments.
- Understand the anatomy of the thoracic outlet, respiratory diaphragm, and pelvic diaphragm and its anatomical attachments.
The Lymphatic System
The lymphatic system allows for the flow of nutrients toward and waste away from individual cells. It is a passive system whose function can be influenced by external forces. Lymph is the substance that leaks out of the arterial capillaries, into the interstitium, and into the single-cell lymphatic vessels. Primary cells of lymph are lymphocytes, which are clear in color, contain proteins, salts, and large particles (such as bacteria and viruses) prior to filtration through a lymph node or organ. Organized lymphatic tissue consists of the spleen and tonsils, for example. Functions include the production of immunologic cells and antibodies, clearing of waste from fighting infections, and filtering toxins.
Lymphatic channels perfuse most of the tissues of the body. Simple squamous epithelium cells of the lymphatic capillaries allow great permeability of fluids from the interstitium back into the lymphatic system. Capillaries flow into larger channels which eventually drain into the venous system via the right lymphatic duct or the thoracic duct. The right upper extremity, right chest, and right upper quadrant of the abdomen drain via the right lymphatic duct. The remaining portions of the body drain into the thoracic duct (sometimes alternatively known as the left lymphatic duct, though this usage is limited).
The functions of the lymphatic system include maintaining fluid balance in the body, purification and cleansing of tissues, defense, and nutrition. Direct external pressures on lymphatic channels increases the flow of lymph. The mechanism of lymphatic flow occurring through lymph channels is influenced by three factors:
- Interstitial fluid pressure: forces fluid into lymphatic capillaries
- Intrinsic lymphatic pumps: channels with valves similar to the venous system that form sections who function independently; Smooth muscle in the channel walls contracts when distended allowing one to pump to the next
- Ionic gradients: fluid goes toward higher concentrations of ions
The eight diaphragms that contribute to lymphatic flow (and its obstruction) are the diaphragm sellae, the tentorium cerebelli (both of which will be discussed in more detail in Chapter 12), the suboccipital diaphragm, the thoracic inlet diaphragm, the respiratory diaphragm, the pelvic diaphragm, the popliteal diaphragm, and the plantar fascia.
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Respiratory diaphragm: |
|
Central tendon | Respiration | Phrenic nerve (C3-C5) | 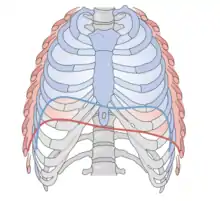 Diaphragm: red - inhalation; blue - exhalation |
The respiratory diaphragm is an important external pump. All movements of internal organs such as respiration and peristalsis affect lymph flow. Movement of the extremities exerts pressure. Respiration causes lymph to move via pressure gradients (negative pressure causes fluid to move toward it; positive pressure pushes it away). The pelvic diaphragm works in synchrony with the abdominal diaphragm to maximize flow of interstitial fluid and lymph, relaxing with contraction of the abdominal diaphragm and springs back with exhalation producing a mechanical pump for the lymphatics in the pelvis and lower abdomen. The ideal order of opening the diaphragms is by opening the thoracic inlet, respiratory diaphragm, pelvic diaphragm, and popliteal diaphragm.
The consequence of decreased lymphatic function is edema, which is the build-up of excess interstitial fluid caused by either too much fluid going into the interstitium or too little getting out. Conditions that overload the interstitium override the absorptive capabilities of the lymphatic system. Excessive interstitial fluid increases interstitial pressure and collapses lymph capillaries resulting in further edema and congestion. Edema also causes dilation of lymph capillaries causing the valves not to function and the intrinsic pump to shut down. Conditions of increased venous pressure are associated with increased capillary filtration rates and tend to produce edema. These include congestive heart failure (both systolic and diastolic), incompetent heart valves, venous obstruction, and gravity. Conditions which decrease osmotic gradients across the capillary, such as cirrhosis and starvation, decrease lymphatic function and lead to edema. Inadequate drainage, such as post-traumatic or
post-surgical scarring will lead to edema. Edema causes compression not only of lymphatic but also vascular and neurological structures, leading to decreased function. Edema causes further fluid stasis which causes a buildup of waste products and a decrease in nutrient delivery. Edema can further affect bioavailability of drugs and hormones, further decreasing function.
Lymphatics Treatment Techniques
Lymphatic techniques can be considered as extensions of myofascial release/soft tissue techniques and should be performed for 30-60 seconds in duration. As discussed in Chapter 2:
| Technique | Direct or indirect | Active or passive | Mechanism of action | Absolute contraindications | Relative contraindications |
|---|---|---|---|---|---|
| Lymphatic | Direct | Passive |
|
|
|
| Myofascial release (MFR) | Direct or indirect | Passive |
|
|
|
Treatment goals of lymphatic techniques include opening myofascial pathways at transitional areas (i.e. diaphragms) of the body, normalizing diaphragmatic motions, increasing pressure differentials to augment fluid flow beyond normal levels, and to mobilize targeted tissue fluids into the lymphatic system. An emphasis on removing impedances to lymphatic flow and improving and augment the flow of lymph is apparent. Techniques which remove somatic dysfunction causing decreased efficiency of respiration, diaphragmatic excursion or motion, or a fascial torsion will improve lymphatic function. The goal is to have a balanced, well-functioning system without edema. The low-pressure lymphatic system is dependent on motion and drainage of lymph for optimal function. These factors are directly treated with osteopathic manipulative medicine. Additionally, fascial torsions can directly decrease lymphatic flow through the fascia. Other techniques include the splenic pump, the liver pump, the pedal pump, effleurage, and petrissage.
Prior to treating any lymphatic issues (i.e. edema), the diaphragms described previously must be opened.
As mentioned previously, the ideal order of opening the diaphragms is by opening the:
- thoracic inlet
- respiratory diaphragm
- pelvic (pre-sacral) diaphragm
- popliteal diaphragm
| Thoracic inlet/outlet release (Steering wheel) | Contact fascia around T1, first rib, and manubrium and take into ease/barrier for myofascial release assessing anterior/posterior motion, translation, and rotation in a clockwise or counterclockwise orientation. To clarify, the landmarks that comprise the thoracic inlet are the manubrium, ribs 1-2, and T1-T4; the thoracic outlet is comprised of the anterior and middle scalenes, the clavicle, and ribs 1-2. |  Thoracic inlet outlet MFR |
|---|---|---|
| Doming of the diaphragm | The patient in the supine position with their thumbs just inferior to the xiphoid process and thenar eminences on the lower costal margin. During a respiration cycle, the physician’s thumbs should follow the diaphragm and move posteriorly. The physician will be able to diagnose restriction of the diaphragm by decreased excursion compared to the other side. Once the patient inhales, the physician should gently resist the motion on the restricted side. With subsequent exhalation, the physician follows the motion of the diaphragm posteriorly and cephalad. |  Doming of Diaphragm |
| Presacral release | The patient in the supine position. The physician makes a C-shape with the thumb, index, and third fingers and presses downward in the lower abdominal region just above the ramus of the pubic bone. As with assessment of the thoracic outlet, compare motion in superior/inferior motion, left and right translation, and torsion (like a steering wheel), looking for fascial restrictions. Direct myofascial release is applied for 30 seconds and a release should be palpated; longer times may be required. |  Pre-sacral Release |
| Popliteal fossa release | The patient supine and the legs extended. The physician's hands assess the popliteal fossa for fascial restrictions in the cephalad, caudad, medial, and lateral directions. |  Popliteal Fossa Release |
| Plantar fascia release - longitudinal stretch | The patient in a supine position. The physician makes a closed fist and places the flat portion of the proximal fifth phalanx against the sole of the patient's foot just proximal to the metatarsal. The flat portion of the physician's proximal phalanges are rolled along the plantar surface toward the calcaneus with moderate pressure contacting the phalanges. |  Plantar Fascia Release - Longitudinal Stretch |
| Plantar fascia release - medial longitudinal arch springing | The patient is supine. The physician places both thumbs under the longitudinal arch of the of the patient's foot. The physician's hands twist in opposite directions in a wringing motion. |  Plantar Fascia Release - Medial Longitudinal Arch Springing |
Once the diaphragms are open, fluid mobilization can be performed.
| Pectoral traction | The patient is supine and the physician places their finger pads inferior to the patient's clavicles at the anterior axillary fold. The physician applies traction to the pectoralis muscles through the axilla following the respiratory cycles. Inhalation with cephalad traction and exhalation with resistance to costal depression is sustained. |  Pectoral Traction |
|---|---|---|
| Thoracic pump (also called the Miller thoracic pump) | The patient is in a prone position. The physician stands at the head of the table with thenar eminences inferior to the patient's clavicles. The patient takes a deep breath and, during exhalation, the physician increases the pressure on the anterior rib cage with each subsequent inhalation and exaggerates exhalation. A rate of 2 compressions per second should be applied. Repeat for 30 seconds. On the last instruction to inhale, the physician suddenly releases the pressure, resulting in the patient taking a very rapid and deep inhalation inflating any atelectatic segments. If the objective is to only increase lymphatic return, the thoracic pump can be performed by continuing to apply the inferior pressure during both inhalation and exhalation, as opposed to only exhalation as was done with the atelectasis component, and there is no sudden release during the last inhalation. |  Thoracic pump |
| Pedal pump (also called the Dalrymple pump) | The patient in the supine position. The physician stands at the foot of the table and plantarflexes the patient's feet (to the comfort level of the patient) while applying a rhythmic alternating pressure to the distal surface of the feet while maintaining plantarflexion. |  Pedal Pump |
| Splenic pump | The patient lies supine and the patient's left hand is abducted to 90 degrees by the physician's right hand. The physician places the left hand over the left costal cartilages overlying the spleen. The left hand exerts pressure directly toward the center of the patient's body in a springing motion with the ribs moving inward. |  Splenic Pump |
| Effleurage | A light stroking motion that is performed by addressing edema and moving in a proximal-to-distal fashion. |  Effleurage - Upper Extremity  Effleurage - Lower Extremity |
| Petrissage | A deeper massaging relative to effleurage (i.e. wringing) onto the muscles is performed in a proximal-to-distal fashion. |  Petrissage - Upper Extremity  Petrissage - Lower Extremity |
Review Questions
1. The lymphatic system handles which of the following substances?
A. Excessive fluid
B. Cellular debris
C. Exudative fluid
D. Bacteria
E. All of the above
2. Which of the following occurs as a direct result of obstructed lymphatic flow?
A. Inflammation
B. Edema
C. Increased circulation to non-obstructed vasculature
D. Neuropathic pain
E. Deep venous thrombosis
3. What is the correct sequence of opening the diaphragms prior to performing a lymphatic technique?
A. the popliteal diaphragm, the pelvic diaphragm, the thoracic inlet/outlet, and the respiratory diaphragm
B. the respiratory diaphragm, the popliteal diaphragm, the thoracic inlet/outlet, and the pelvic diaphragm
C. the thoracic inlet/outlet, the respiratory diaphragm, the pelvic diaphragm, and the popliteal diaphragm
D. the respiratory diaphragm, the pelvic diaphragm, the thoracic inlet/outlet, and the popliteal diaphragm
E. the thoracic inlet/outlet, the respiratory diaphragm, the popliteal diaphragm, and the pelvic diaphragm
4. A 13-year-old male presents to his pediatrician with his mother for evaluation of worsening asthma symptoms. He initially was having 1-2 episodes per week but his symptoms have progressed to occurring every day despite treatment with an albuterol inhaler and montelukast. Before adding any other medications to his regimen, his mother wanted to attempt treatment with osteopathic manipulative medicine. His medical history is unremarkable aside from his moderate reactive airway disease. His medications include albuterol inhaler (used as needed) and montelukast daily. His vital signs are stable and afebrile. He has coarse breath sounds diffusely and bilaterally and faint wheezing. The remainder of his physical exam is unremarkable. His structural exam reveals the following:
- C3-C5 RLSR
- Hypertonic scalene, sternocleidomastoid, and trapezius muscles
- Thoracic paraspinal muscle hypertonicity
- T1-T4 NSLRR
- Ribs 3-5 exhalation dysfunction on the right
- Left hemidiaphragm restriction
Which of the following is the best initial treatment for this patient?
A. Treatment of the thoracic dysfunctions
B. Treatment of the rib dysfunctions
C. Treatment of the hypertonic musculature
D. Treatment of the cervical dysfunctions
E. Treatment of the diaphragm restriction
5. A 79-year-old female presents to her primary care physician complaining of shortness of breath. Her medical history is notable for coronary artery disease, chronic systolic heart failure with ischemic cardiomyopathy and an ejection fraction of 45%, hypertensive heart and kidney disease, chronic kidney disease stage 3, hyperlipidemia, diabetes mellitus type 2, and osteoporosis. Her symptoms began 1 week ago. She notes worsening fatigue and shortness of breath from her baseline. She is now having shortness of breath at rest. She states she slept in her recliner last night. She notes an 8-pound weight gain over the last week. Her vital signs show temperature of 99 F, heart rate of 104 bpm, respiratory rate of 22 bpm with shallow breaths, blood pressure of 150/98, and oxygen saturation of 91% on room air. Her physical exam reveals a 2/6 systolic murmur over the left upper sternal border and decreased breath sounds at bilateral lung bases with bilateral rales and wheezes throughout. The remainder of her physical exam is unremarkable for her age. Her osteopathic structural exam reveals:
- boggy suboccipital tissues
- T1-T4 NRRSL
- hypertonic paraspinal muscles in over the levels of T1-T5
- inhalation restriction of ribs 10-12
- decreased bilateral diaphragmatic excursion
Which of the following treatment techniques could be utilized in the management of this patient after opening the appropriate diaphragms?
A. The physician stands at the head of the table with the thumbs and fingers above the bilateral clavicles and applying a gentle caudad pumping motion at a rate of 2 pumps per second.
B. The physician stands at the head of the table with the thumbs and fingers on the bilateral clavicles and applying a gentle caudad pumping motion at a rate of 2 pumps per second.
C. The physician stands at the head of the table with the thumbs and fingers below the bilateral clavicles and applying a gentle caudad pumping motion at a rate of 2 pumps per second.
D. The physician stands at the foot of the bed the hands on distal plantar aspect of patient's feet with gentle dorsiflexion applied; a gentle cephalad pumping motion at a rate of 2 pumps per second.
E. The physician stands at the foot of the bed the hands on proximal plantar aspect of patient's feet with gentle dorsiflexion applied; a gentle cephalad pumping motion at a rate of 2 pumps per second.
Answers to Review Questions
- E
- B
- C
- A
- C