Chapter 8: Sacrum and Pubic
Objectives:
- Identify pelvic and sacral landmarks and ligaments to diagnose sacral somatic dysfunction.
- Document sacral somatic dysfunction with appropriate nomenclature.
- Understand and apply the relationship between L5 and sacral dysfunctions.
- Treat sacral and pubic somatic dysfunctions.
Sacrum Anatomy
The anatomy of the sacrum and pubic regions was introduced previously in Chapter 7.
The sacrum begins as 5 unfused vertebrae at birth. Initial fusion begins around age 16 and completes by age 26. It is a major load bearing structure, serving as the base of the spine and the trunk. It is suspended in place between the ilia. The ligament which joins the sacrum to the ilia is the sacroiliac ligament.
The sacrum is composed of five fused vertebrae. The anterior portion of the first segment (S1) is referred to as the sacral promontory. Sacral somatic dysfunction diagnoses are named by motion at the sacral promontory. The sacral base is the top (most cephalad) part of the sacrum. In somatic dysfunctions, the sacral base can be identified as being shallow (or posterior) or deep (or anterior). The sacral apex is the bottom part of the sacrum, which articulates with the coccyx. The sacral sulci (or sacral bases) are located on the superior lateral part of the sacrum. They are identified as being posterior (or shallow) or anterior (or deep) in somatic dysfunctions. The inferior lateral angles (ILAs) of the sacrum are located at the inferior lateral part of the sacrum. They are identified as being shallow (or posterior), deep (or anterior), superior or inferior in somatic dysfunctions. The innominates articulate with the femur at the acetabulum, the sacrum at the SI joint, and the pubic bones articulate with each other at the pubic symphysis. The articular process is where the sacrum articulates with L5. These two arms join at S2. Nerve roots exit through the sacral foramina.
There are four important ligaments to identify when considering pelvis anatomy:
- the iliolumbar ligament is a broad ligament that stabilizes L5 and anterior motion of the lower lumbar spine;
- the anterior sacral ligament (sacroiliac ligament) connects the sacrum to the innominates;
- the sacrospinous ligament connects the sacrum to the ischial spine; and
- the sacrotuberous ligament which connects the sacrum to the ischium.
The sacrospinous and sacrotuberous ligaments restrict sacral flexion and posterior innominate rotation. The sacroiliac ligament is contiguous with the sacrotuberous ligament.
There are three significant muscles which attach the sacrum: the gluteus maximus, the multifidus, and the piriformis. The gluteus maximus is the primary extensor and abductor of the hip and attaches to the posterior aspect of the sacrum. When the sacrum is pulled posteriorly, the gluteus maximus is used due to its posterior attachment site. The multifidus coalesces into a thicker muscle as it descends inferiorly and attaches to the sacrum posteriorly as well. On the anterior surface, the piriformis attaches and serves as an external rotator of the hip. When the sacrum is pulled forward, the piriformis is used due to its anterior attachment site. The piriformis is the only muscle to attach to the anterior surface of the sacrum.
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Piriformis | Anterior surface of the sacrum | Greater trochanter of the femur | Hip: external rotation, abduction, and extension | Sacral plexus (L5-S2) | 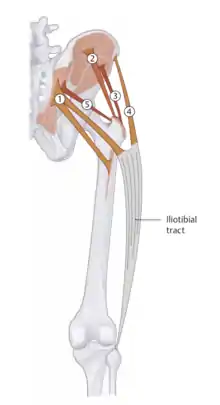 5 - Piriformis |
| Gluteus maximus | Lateral part of the dorsal surface of the sacrum, posterior part of the gluteal surface of the ilium, from the thoracolumbar fascia, and the sacrotuberous ligament |
|
Extend and externally rotate the hip as well as stabilize the hip in both the sagittal and coronal planes (entire muscle); adduction (upper fibers); adduction (lower fibers) | Inferior gluteal nerve (L5-S2) | 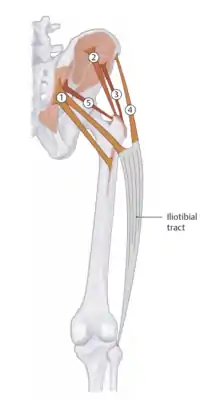 1 - Gluteus maximus |
With regard to the neuroanatomy of the sacral region, the spinal cord ends at the level of L2, below which the conus medullaris begins and the cauda equina follows to the level of S4. The dura matter ends at the level of S2; dura mater attachments will be the subject of Chapter 14 but are, briefly, the surfaces of the OA, C2, C3, and S2 vertebrae.
The pelvic splanchnic nerves exit from the S2-S4 nerve roots and are responsible for parasympathetic innervation of the viscerosomatic reflexes discussed in Chapter 11.
There are four types of sacral motion: respiratory motion, craniosacral motion, postural motion, and dynamic motion. The axes of motion of the sacrum are shown in Figure 8.1. During respiration and craniosacral motion, the sacral base will move posteriorly about the superior transverse axis, passing through the level of S2. Postural motion occurs during ambulation, utilizing the middle transverse axis (S3). Innominate rotation occurs about the inferior transverse axis (S4). The left and right oblique axis are utilized during the dynamic motion of ambulation; when bearing weight on the left leg, the left oblique axis is engaged.
Sacrum Somatic Dysfunctions
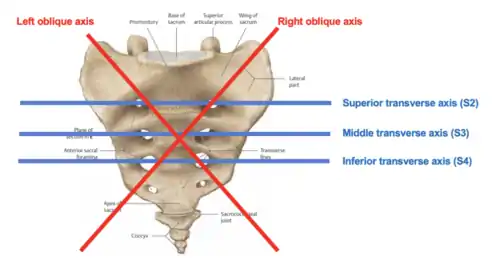
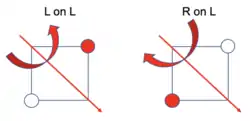
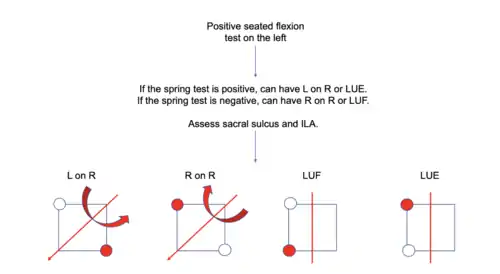
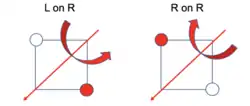
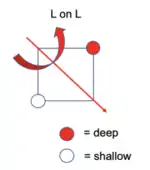
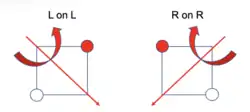
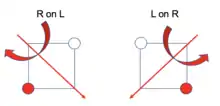
Sacrum nomenclature is always named with the sacral promontory as a point of reference. Torsional axes are always named by the SI joint involved. Torsion dysfunctions are named by rotation on axis. For example, a right on left sacral somatic dysfunction means that a rightward rotation is occurring about a left oblique axis.
Left on left and right on right sacral somatic dysfunctions are considered anterior torsions because the dysfunction involves moving the base of the sacrum forward and are termed physiologic because they occur normally during gait. Right on left and left on right sacral somatic dysfunctions are termed posterior torsions because the sacral base is moving posteriorly and are termed non-physiologic because they do not occur during gait (i.e. physiologic conditions).
With respect to sacral shear somatic dysfunctions, these are always pathologic and related to some type of trauma. They are uncommon. Unilateral shear somatic dysfunctions occur when one half of the sacrum is pulled in one direction; bilateral shear somatic dysfunctions occur when both halves of the sacrum are pulled in a direction. These dysfunctions are the result of abnormal motion around a transverse axis. Shear dysfunctions occur either in a flexion or extension motion.
The four possible sacral shear somatic dysfunctions are:
- unilateral sacral flexion dysfunction
- unilateral sacral extension dysfunction
- bilateral sacral flexion dysfunction
- bilateral sacral extension dysfunction
Lumbosacral mechanics are next to be considered because L5 and the sacrum always move in opposite directions under physiologic conditions to compensate for motion of the lumbar spine and the opposing motions of the sacrum. Sacral extension is known as counternutation and sacral flexion is known as nutation.
The following observations can be used to predict lumbar and sacral dysfunctions:
- If L5 is sidebent, the sacral oblique axis is engaged on the same side as the sidebending.
- If L5 is rotated, the sacrum rotates the opposite way on an oblique axis.
Examples:
| Lumbar and sacral dysfunctions | Conclusions |
|---|---|
| Case #1: L5 FRRSR |
Sacrum will be rotated left (opposite side of rotation) on a right oblique axis (same side as sidebending) – this is a L on R torsion. |
| Case #2: L5 NSLRR |
Sacrum will be rotated left (opposite side of rotation) on a left oblique axis (same side as sidebending) – this is an L on L torsion. |
| Case #3: L on R torsion |
|
| Case #4: L on L torsion |
|
Conclusion: Type 1 dysfunctions are anterior torsions and type 2 dysfunctions are posterior torsions.
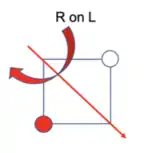
In order to diagnose a sacral somatic dysfunction, three of any of the four following pieces of information are required:
- Seated flexion test findings
- Spring test findings
- Sacral sulcus depth findings
- Inferior lateral angle position findings
A freely-moving sacroiliac joint will allow for full lumbar flexion before locking and rotating the pelvis forward. The seated flexion test, as discussed in prior chapters, is utilized because a dysfunctional sacroiliac joint will lock earlier and rotate the pelvis forward first. Sitting stabilizes the innominates and allows isolation of sacral motion.
| The seated flexion test is performed to also determine laterality of sacroiliac dysfunction. It is done by having the patient seated on the exam table with the knees flexed to 90 degrees. The physician sits behind the patient with the eyes at the level of the pelvis and the thumbs on the PSIS. The patient is asked to bend forward. Ideally, the patient’s feet should be in contact with the ground while performing this test to avoid injury to the patient. As with the standing flexion test, the side that moves first and moves the furthest is the positive side, indicating sacroiliac restriction on the ipsilateral side. |  Seated flexion test |
A freely-moving sacrum should have recoil when it is directly compressed. A positive spring test occurs when direct compression of the sacrum in the Sphinx position has no recoil and feels rigid (“no spring”); it also indicates posterior displacement of the sacral base.
 Spring Test |
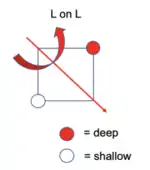
The positions of the sacral sulcus and the inferior lateral angle are based on static examination and palpation of the sacrum. The sacral sulcus is described as being either deep or shallow based on sacral base positioning; it corresponds to the distance between the PSIS and the sacral base. The inferior lateral angle is described as posterior or anterior based on sacral apex positioning.
 Sacral Landmark Depths |
There are ten possible sacrum somatic dysfunctions summarized in Table 8.1.
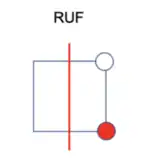
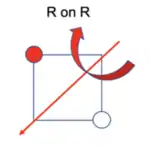
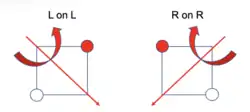
| Sacral somatic dysfunction | Positive seated flexion side | Spring test | Sacral sulcus deep | ILA shallow | Visual representation |
|---|---|---|---|---|---|
| Left on left (L on L) | Right | Negative | Right | Left |  L on L |
| Right on right (R on R) | Left | Negative | Left | Right | 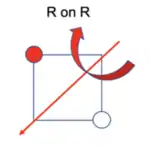 R on R |
| Left on right (L on R) | Right | Positive | Right | Left | 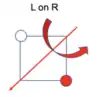 L on R |
| Right on left (R on L) | Left | Positive | Left | Right | 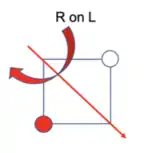 R on L |
| Right unilateral flexion (RUF) | Right* (false positive) | Negative | Right | Right | 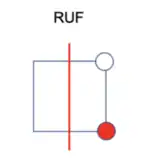 R Unilateral Flexion |
| Left unilateral flexion (LUF) | Left* (false positive) | Negative | Left | Left | 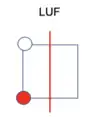 L Unilateral Flexion |
| Right unilateral extension (RUE) | Right* (false positive) | Positive | Left | Left | 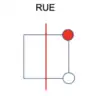 R Unilateral Extension |
| Left unilateral extension (LUE) | Left* (false positive) | Positive | Right | Right | 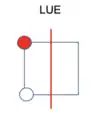 L Unilateral Extension |
| Bilateral flexion | False negative | Negative (false negative) | Both | Both | |
| Bilateral extension | False negative | Positive | Neither | Neither |
Worked Examples of Sacrum Diagnoses
Sacral somatic dysfunction diagnoses:
- What side is the seated flexion test positive on?
- What does the spring test show?
- What are the relative positions of the sacral sulcus and inferolateral angles?
| Example: Sacral diagnosis possibilities from seated flexion test |
|---|
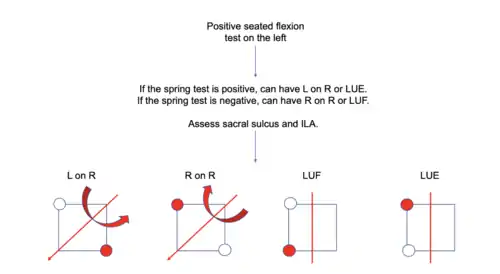 Positive Seated Flexion Test on the Left 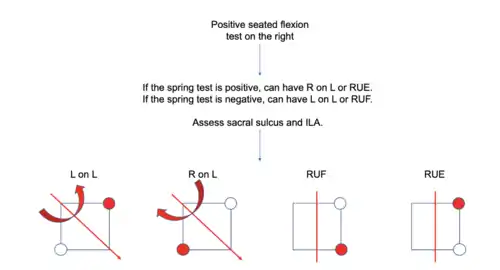 Positive Seated Flexion Test on the Right |
| Example #1 |
|---|
Structural examination findings for a patient reveal the following:
|
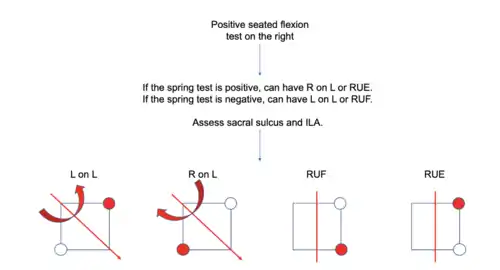 Positive Seated Flextion Test on Right |
|
Seated Flexion Test is positive on the right:
|
|
Spring test is negative
|
|
Sacral sulcus is deep on the right. Inferior lateral angle (ILA) is shallow on the right.
 Right Unilateral Flexion |
| Example #2 |
|---|
Structural examination findings for a patient reveal the following:
|
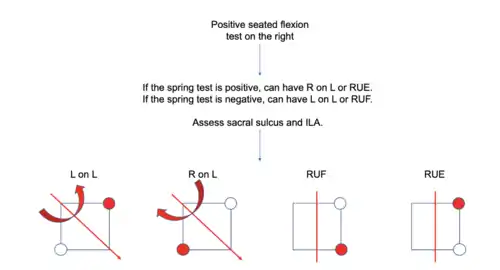 Positive Seated Flextion Test on Right |
|
Seated Flexion Test is positive on the right:
|
|
Spring test is not provided. |
|
Sacral base is deep on the left. ILA is shallow on the right.
|
 R on L |
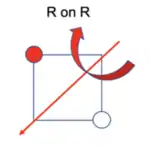
| Example #3 |
|---|
Structural examination findings for a patient reveal the following:
|
 Positive Seated Flextion Test on Left |
|
Seated Flexion Test is positive on the right:
|
|
Spring test is not provided. |
|
Sacral base is deep on the left. ILA is shallow on the left.
 Example 3 Possibilities
|
 R on R |
| Example #4 |
|---|
Structural examination findings for a patient reveal the following:
|
|
Seated Flexion Test is not given. |
|
Spring test is negative.
|
|
Sacral base is deep on the left. ILA is shallow on the left.
 Example 4 Possibilities
|
 R on R |
| Example #5 |
|---|
Structural examination findings for a patient reveal the following:
|
|
Seated flexion test is positive on the right.
|
|
Spring test is negative.
|
|
Sacral sulcus is not given. ILA is shallow on the left.
 L on L
|
 L on L |
Treatment of Sacrum Somatic Dysfunctions
Sacral torsion dysfunctions can be treated with post-isometric relaxation muscle energy:
| Anterior Torsions (i.e. Left on Left or Right on Right) | The mnemonic to remember treatment of these dysfunctions is Up, Up, Up, or Down, Down, Down. The three directions in the mnemonic refer to which way the patient’s torso faces, the side of the dysfunctional axis is placed, and which direction the physician force is directed, respectively.
 Anterior Torsions |
| Up, Up, Up: Place the patient in lateral recumbent position with dysfunctional axis side up. Keeping the pelvis in recumbent, swivel only the patient’s upper body into supine position until motion is felt over the restricted sacral base (the sacral sulcus closer to the table). Flex the patient’s bilateral hips until motion is felt over the restricted sacral base. Keeping the knees also flexed, and the weight of the patient’s legs supported by the physician’s body, lift both lower extremities off the table until the restrictive barrier is reached at the restricted sacral base. The patient contracts their gluteus maximus by pushing their lower extremities downward into the table, and this force is met by the physician to produce an isometric contraction. |  Up Up Up |
| Down, Down, Down: Place the patient in lateral recumbent position with dysfunctional axis side down. Keeping the pelvis in recumbent, swivel the patient’s upper body into prone position until motion is felt at the restricted sacral base (the sacral sulcus that is higher). Flex the patient’s bilateral hips until motion is felt over the restricted sacral base. Keeping the knees also flexed, Lower both lower extremities off the table until the restrictive barrier is reached at the restricted sacral base. The patient contracts their gluteus maximus by pushing their lower extremities upwards towards the table, and this force is met by the physician to produce an isometric contraction. |  Down Down Down |
| Posterior Torsions (i.e. Right on Left or Left on Right) | Using the same mnemonic convention as anterior torsions, the treatment technique for posterior torsions is either Up, Down, Down, or Down, Up, Up.
 Posterior Torsions |
| Up, Down, Down: Place the patient in lateral recumbent position with dysfunctional axis side down. Keeping the pelvis in recumbent, swivel the patient’s upper body into supine position until motion is felt at the restricted sacral base (the sacral sulcus that is higher). Flex the patient’s hip on the side of the restricted sacral base until motion is felt over the restricted sacral base. Keeping the knee also flexed, lower the lower extremity off the table until the restrictive barrier is reached at the restricted sacral base. The patient contracts their piriformis muscle by pushing their lower extremity upwards towards the table, and this force is met by the physician to produce an isometric contraction. | 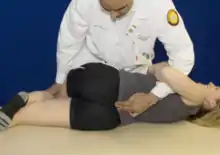 Up Down Down |
| Down, Up, Up: Place the patient in lateral recumbent position with dysfunctional axis side up. Keeping the pelvis in recumbent, the swivel the patient’s upper body into prone position until motion is felt at the restricted sacral base (the sacral sulcus that is towards the table). Flex the patient’s hip on the side of the restricted sacral base until motion is felt over the restricted sacral base. Lifting up on the medial/lateral malleoli, the raise the lower extremity off the table until the restrictive barrier is reached at the restricted sacral base. The patient contracts their piriformis muscle by pushing their lower extremity downwards towards the table, and this force is met by the physician to produce an isometric contraction. |  Down Up Up |
Sacral shears (unilateral flexion shears, unilateral extension shears, bilateral flexion shears, and bilateral extension shears) use respiratory motion of the sacrum in combination with direct physician force to correct sacral positioning. These techniques require that the sacroiliac joint be in a gapped position in order to be effective. Sacral shear dysfunctions can be treated with respiratory-assisted muscle energy:
| Unilateral Flexion Shear: Place the patient in the prone position on the table. Abduct and internally rotate the entire lower extremity on the dysfunctional side until the ilium is as laterally displaced as possible with respect to the sacrum. Contact the inferior lateral angle on the dysfunctional side. Instruct the patient to perform 3 long, slow cycles of inhalation and exhalation. During the patient’s inhalation phase, apply firm downward pressure onto the inferior lateral angle. During the patient’s exhalation phase, actively resist sacral nutation. | 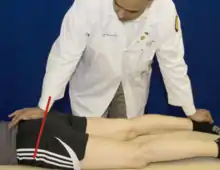 Unilateral Flexion Shear ME |
| Unilateral Extension Shear: Place the patient in the prone Sphinx position on the table. Abduct and internally rotate the entire lower extremity on the dysfunctional side until the ilium is as laterally displaced as possible with respect to the sacrum. Contact the base of the sacrum on the dysfunctional side. Instruct the patient to perform 3 long, slow cycles of inhalation and exhalation. During the patient’s exhalation phase, apply firm downward pressure onto the sacral base. During the patient’s inhalation phase, actively resist sacral counternutation. | 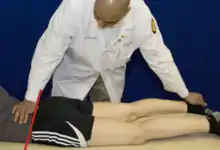 Unilateral Extension Shear ME |
| Bilateral Flexion Shear: Place the patient in the prone position on the table. Abduct and internally rotate both lower extremities until the ilia are as laterally displaced as possible with respect to the sacrum. Contact the inferior lateral angles of the sacrum. Instruct the patient to perform 3 long, slow cycles of inhalation and exhalation. During the patient’s inhalation phase, apply firm downward pressure onto the inferior lateral angles. During the patient’s exhalation phase, actively resist sacral nutation. |  Bilateral Flexion Shear ME |
| Bilateral Extension Shear: Place the patient in the prone Sphinx position on the table. Abduct and internally rotate both lower extremities until the ilia are as laterally displaced as possible with respect to the sacrum. Contact the base of the sacrum in the midline. Instruct the patient to perform 3 long, slow cycles of inhalation and exhalation. During the patient’s exhalation phase, apply firm downward pressure onto the sacral base. During the patient’s inhalation phase, actively resist sacral counternutation. |  Bilateral Extension Shear ME |
Anatomy of the Pubic Region
The pelvic girdle is made of the two innominates and the sacrum. There are differences in the angles between the android male pelvis (acute, ca. 70o) and the gynecoid female pelvis (obtuse, ca. 100o). The gynecoid pelvis has increased flaring of the ilia. The android pelvis is heavier and has more pronounced muscle attachment; the ischial tuberosities are closer in the android pelvis than in the gynecoid pelvis, and the pelvis outlet is thus comparatively smaller. All of the ilia are less flared in the android pelvis than in the gynecoid pelvis, so the greater pelvis is deeper. The pelvic inlet is heart-shaped in the android pelvis and more transversely oval in the gynecoid pelvis. The gynecoid pelvis is broader than in the android pelvis to allow the passage of the fetal head.
The pelvic diaphragm (interchangeably called the pelvic floor) is often overlooked as a source of pain. It may be the cause of lower back pain but is not often considered as the first issue. It serves as a major crossroads for blood, lymph, and nerves and is closely connected to the abdominal diaphragm. Most dysfunctions of the pelvic diaphragm occur in females during pregnancy. The muscles of the pelvic diaphragm include the levator ani (composed of the puborectalis, the pubococcygeus, and the iliococcygeus) and the coccygeus. The piriformis and the coccygeus form the posterolateral aspects of the pelvic floor. The ischial tuberosity serves as a landmark for treating pelvic floor dysfunctions. To contact the pelvic diaphragm, the physician will palpate through a significant amount of connective tissue and adipose. Once a firm feeling is palpated, contact is made. The pelvic diaphragm will move with the respiratory cycle and tighten with inspiration.
The pubic symphysis is a dense fibrocartilaginous joint. Under physiologic conditions, the pubic tubercles should be less than 1 cm apart; the symphysis has the inherent ability to move ca. 2 mm superiorly or inferiorly during the gait cycle. Rotation is limited to 1-2o. The major function of the pubic symphysis is force distribution. During pregnancy, the pubic symphysis becomes relaxed.
To locate the pubic symphysis:
- The patient is supine.
- Palpating with the thenar and hypothenar eminences starting from the umbilicus working towards the pelvis. The physician's fingers are arched off of the patient’s body. As the physician moves distally, the thenar and hypothenar eminence will locate the pubic symphysis by feeling a bony prominence.
- Once located, stay midline and place one thumb on one pubic tubercle and the other thumb on the other pubic tubercle. Make sure to be on the same anatomical location on each side. For example, palpate the superior margin of the tubercle with each hand. The physician should not have one thumb on the superior margin and one on the inferior margin. This skews the diagnosis when evaluating for symmetry. The physician evaluates the heights (inferior or superior) of the pubic tubercles. The physician then assesses for tenderness over the pubic symphysis midline.
To diagnose a pubic somatic dysfunction, use the ASIS compression test or standing flexion test to evaluate for the side of most restriction. Once determined, this will be the side that has dysfunction. Note that the ASIS compression test evaluates the pubic bones, innominates and SI joint, therefore, keep in mind there may be a combination of dysfunctions.
| Diagnosis | Pubic symphysis | Left pubic tubercle | Right pubic tubercle |
|---|---|---|---|
| Pubic compression | Tender | Symmetric | Symmetric |
| Gapped symphysis | Widened | Symmetric | Symmetric |
| Left superior pubic shear | Tender | Superior | Midline |
| Left inferior pubic shear | Tender | Inferior | Midline |
| Right superior pubic shear | Tender | Midline | Superior |
| Right inferior pubic shear | Tender | Midline | Inferior |
| Example: Diagnosing a pubic dysfunction |
|---|
| The following static findings are palpated: a positive standing flexion test on the right, ASIS lower on the right, PSIS higher on the right, longer leg on the right, and the right pubic tubercle is tender and inferior to that on the left. The diagnosis is a right inferior pubic shear dysfunction based on these findings. |
Treatment of Pubic Somatic Dysfunctions
Somatic dysfunctions of the pubic symphysis include superior pubic shear dysfunctions, inferior pubic shear dysfunctions, gapped pubic dysfunctions, and compression pubic dysfunctions. Pubic somatic dysfunctions are relatively uncommon. Superior shear dysfunctions mirror posterior innominate dysfunctions; Inferior shear dysfunctions mirror anterior innominate dysfunctions. Superior and inferior shear dysfunctions are caused by trauma or hypertonic adductors respectively. (Other muscles which may be involved in pubic symphysis dysfunctions include the pectineus, gracilis, and rectus abdominus.)
For treatment of pubic symphysis dysfunctions using post-isometric relaxation muscle energy:
| Gapped Pubic Symphysis (utilizes hip abductors): Patient is supine, with knees bent and knees apart. The physician places their hands on the lateral aspect of each of the patient’s knees. The physician asks the patient to push out into their hands and at the same time the operator resists this motion resulting in no movement of the legs. For the second and third iterations, the physician brings the knees closer together. |  Gapped Pubic Symphysis ME |
| Compressed Pubic Symphysis (utilizes hip adductors): Patient is supine, with knees bent and knees together. The physician places their fist in between the patient’s knees. The physician asks the patient to push into their hand and at the same time the physician resists this motion resulting in no movement of the legs. For the second iteration, the physician places two fists between the knees; for the final iteration, the physician places the forearm between the knees. |  Compressed Pubic Symphysis ME |
For treatment of pubic shear dysfunctions using muscle energy, treatment involves:
- contraction to relax the adductors by gapping the pubic symphysis using the compression technique described previously
- treatment of the pubic shear according to its corresponding analogous innominate dysfunction (using the hamstrings for inferior shear dysfunction and using the quadriceps for superior shear dysfunction)
- contraction to relax the abductors by compressing the pubic symphysis using the gapping technique described previously
| Inferior Pubic Shear: The patient is supine. The physician gaps the pubic symphysis using the compression technique. The physician stands on the side of the dysfunction. The patient’s leg is flexed until a restrictive barrier is contacted. Once at that barrier, the patient is instructed to push back against the physician. The physician resists this motion resulting in no movement. The patient's leg is brought further into flexion during each iteration of the treatment. Lastly, the physician compresses the pubic symphysis using the gapping technique. |  Inferior Pubic Shear ME |
| Superior Pubic Shear: The patient is supine. The physician gaps the pubic symphysis using the compression technique. The physician stands on the side of the dysfunction. The patient’s leg is extended until a restrictive barrier is contacted. Once at that barrier, the patient is instructed to push back against the physician. The physician resists this motion resulting in no movement. The patient's leg is brought further into extension during each iteration of the treatment. Lastly, the physician compresses the pubic symphysis using the gapping technique. |  Superior Pubic Shear ME |
Review Questions
Questions 1-6: Match the sacrum diagnosis based on the following static findings (choices may be used more than once):
1. Pain present over the pubic symphysis with superior displacement of the left pubic tubercle.
2. Positive seated flexion test on the left. Spring test is negative. Sacral sulcus is deep on the left. Inferior lateral angle (ILA) is shallow on the left.
3. Positive seated flexion test on the right. Sacral base deep on the left. ILA is shallow on the right.
4. Positive seated flexion test on the right. Sacral base shallow on the right. ILA is deep on the right.
5. Positive seated flexion test on the left. Sacral base is deep on the right. ILA is deep on the left.
6. Positive seated flexion test on the right. Spring test is negative. ILA is shallow on the left.
A. Right on right sacral torsion
B. Left on left sacral torsion
C. Right on left sacral torsion
D. Left on right sacral torsion
E. Right unilateral sacral flexion
F. Right unilateral sacral extension
G. Left unilateral sacral flexion
H. Left unilateral sacral extension
I. Bilateral sacral flexion
J. Bilateral sacral extension
K. Right superior pubic shear
L. Right inferior pubic shear
M. Left superior pubic shear
N. Left inferior pubic shear
7. Where should the physician's force be directed muscle energy treatment of a patient with a right unilateral sacral flexion somatic dysfunction?
A. Right sacral apex
B. Right sacral base
C. Left sacral apex
D. Left sacral base
E. At the lumbosacral junction
8. An anterior sacral torsion, such as a left on left or right on right sacral somatic dysfunction, is treated with muscle energy using the ____ muscle. A posterior sacral torsion, such as a right on left or a left on right sacral somatic dysfunction, is treated with muscle energy using the ____ muscle.
A. gluteus maximus; gluteus maximus
B. piriformis; gluteus maximus
C. gluteus maximus; piriformis
D. piriformis; piriformis
9. What is the correct sequence for treating a pubic shear?
A. Bilaterally contract the abductors, treat the shear, bilaterally contract the adductors
B. Treat the shear, bilaterally contract the adductors, bilaterally contract the abductors
C. Bilaterally contract the abductors, bilaterally contract the adductors, treat the shear
D. Bilaterally contrast the adductors, treat the shear, bilaterally contract the abductors
E. Treat the shear, bilaterally contract the abductors, bilaterally contract the adductors
F. Bilaterally contract the adductors, bilaterally contract the abductors, treat the shear
10. Which of the following statements is true regarding sacral motion about the respective segmental level?
A. The superior transverse axis is about S3.
B. The sacral base moves posteriorly during respiration about S2.
C. Innominate motion occurs about the middle transverse axis.
D. Postural motion occurs around the inferior transverse axis.
E. The left and right oblique axes are engaged during hip flexion and extension.
11. The motion of which anatomic landmark is used to diagnose sacral somatic dysfunctions?
A. Sacral sulcus
B. Inferior lateral angle
C. Sacral promontory
D. Sacral apex
E. Sacral base
12. Which of the following statements regarding pubic dysfunctions is correct?
A. Pubic somatic dysfunctions are fairly common.
B. Superior pubic shear dysfunctions are caused by hypertonic quadriceps muscles.
C. Inferior pubic shear dysfunctions mirror anterior innominate dysfunctions.
D. Superior pubic shears are less often caused by trauma than hypertonic musculature.
Answers to Review Questions
- M
- G
- C
- F
- H
- B
- A
- C
- D
- B
- C
- C