Chapter 13: Neuroanatomy Primer
Objectives:
- Perform a neurological evaluation as part of an Osteopathic Structural Exam
- Perform and document muscle strength testing of the upper and lower extremities
- Perform and document deep tendon reflex testing of the upper and lower extremities
- Perform sensation testing and understand the sensory dermatome map
- Describe and understand the neuroanatomy of the brachial plexus
- Describe and understand the neuroanatomy of the lumbosacral plexus
Neurological Evaluation
Neurological evaluation should be a standard part of any osteopathic structural examination.
It involves:
- muscle strength testing
- sensation testing, and
- deep tendon reflex testing
Muscle Strength Testing
Muscle strength testing involves testing muscle groups for weakness or asymmetry of strength. Strength is graded on a scale from 0 to 5:
| Score | Interpretation |
|---|---|
| 0/5 | No contraction |
| 1/5 | Palpable or visible contraction |
| 2/5 | Active movement, full range of motion, no gravity |
| 3/5 | Active movement, full range of motion, against gravity |
| 4/5 | Active movement, full range of motion, against gravity and normal resistance |
| 5/5 | Exert sufficient resistance considered normal if no inhibiting factors are present |
Muscle strength testing is performed bilaterally for the upper and lower extremities. If weakness if present, both sides should be compared. Causes of asymmetric muscle strength are multifactorial but not limited to a cerebrovascular accident (a stroke) or other neurologic pathology.
Muscle strength testing of the upper extremity is done by assessing spinal levels C5-T1 through the following motions against resistance with the patient seated:
| Spinal level | Motions |
|---|---|
| C5 | Elbow flexion |
| C6 | Wrist extension |
| C7 | Wrist flexion |
| C8 | Curling of the fingers |
| T1 | Finger abduction/adduction |
Muscle strength testing of the lower extremity is done by assessing spinal levels L2-S1 through the following motions against resistance with the patient seated:
| Spinal level | Motions |
|---|---|
| L2 | Hip flexion (knee to the ceiling) |
| L3 | Knee extension (knee kick forward) |
| L4 | Knee flexion (knee pulled backward from extension) |
| L5 | Great toe extension (great toe toward the ceiling) |
| S1 | Plantarflexion ("pushing on the gas pedal") |
Deep Tendon Reflexes
Deep tendon reflex testing involves placing the physician’s thumb on the belly of the muscle and striking it with a reflex hammer and observing the movement of the reflex being tested. Strength is graded on a scale from 0 to 4 (score may see listed as 2/4 or 2+, see below):
| Score | Interpretation |
|---|---|
| 0/4 | No response; absent |
| 1/4 | Diminished; hypoactive |
| 2/4 | Normal tone |
| 3/4 | Brisker than average; hyperactive |
| 4/4 | Very brisk; clonic; sustained |
- The biceps reflex (C5 nerve root) is elicited by the physician placing the thumb on the biceps tendon and striking the thumb with the reflex hammer and observing the arm movement. This is repeated and compared with the other arm.
- The brachioradialis reflex (C6 nerve root) is observed by striking the brachioradialis tendon directly with the hammer when the patient's arm is resting. Strike the tendon roughly 3 inches above the wrist. Note the reflex supination. Repeat and compare to the other arm.
- The triceps reflex (C7 nerve root) is measured by striking the triceps tendon directly with the hammer while the physician is holding the patient's arm with the opposite hand. Repeat and compare to the other arm.
- The patellar reflex (L4 nerve root) is performed by the lower leg hanging freely off the edge of the bench, the knee jerk is tested by striking the quadriceps tendon directly with the reflex hammer. Repeat and compare to the other leg.
- The ankle reflex (S1 nerve root) is elicited by the physician holding the relaxed foot with one hand and striking the Achilles tendon with the hammer and noting plantar flexion.
Sensory Dermatomes
Sensation testing is utilized to assess pain, light touch, and proprioception. A dermatome is an area of the skin that is supplied by a branch of a single spinal nerve root. Dermatomes may not correspond precisely to Figure 13.1, but the key sensory points are identified.

Figure 13.1 - Sensory dermatomes
Neuroanatomy of the brachial plexus
This section was modified from https://accessphysiotherapy.mhmedical.com/data/Multimedia/grandRounds/brachial/media/brachial_print.html
The brachial plexus innervates the pectoral girdle and the upper limb, with contributions from the ventral rami of spinal nerves at the levels of C5 through T1. The nerves that form this plexus originate from the trunks and cords. Trunks are large bundles of axons contributed by several spinal nerves. Cords are smaller branches that originate at trunks. Both trunks and cords are named according to their location relative to the axillary artery, a large artery supplying the upper limb. Therefore, we have superior, middle, and inferior trunks and lateral, medial, and posterior cords.
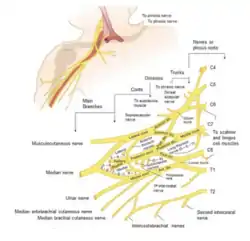
Figure 13.2 - Brachial plexus
The six divisions that terminate from the brachial plexus are the musculocutaneous nerve, the axillary nerve, the radial nerve, the median nerve, the ulnar nerve, and the thoracodorsal nerve. Moving distally, the lateral cord forms the musculocutaneous nerve and, together with the medial cord, forms the median nerve. The posterior cord nerve branches will form the axillary nerve, the radial nerve, the thoracodorsal nerve, and the subscapular nerve. The medial cord also gives rise to the ulnar nerve.
The musculocutaneous nerve innervates the biceps, brachialis, and coracobrachialis. The biceps brachii muscle is a flexor of the shoulder and elbow and a supinator of the forearm. To understand its full function, envision a man driving a corkscrew into a bottle of wine (supinating), pulling out the cork (elbow flexion), and drinking the wine (shoulder flexion). Sensation is provided to the lateral surface of the forearm through the lateral antebrachial cutaneous nerve branch.
The axillary nerve innervates the deltoid and the teres minor. The deltoid is a three-part muscle: the anterior deltoid flexes, the middle deltoid abducts, and the posterior deltoid extends the shoulder. Of the three motions, the deltoid acts most powerfully in abduction. The C5 neurologic level supplies sensation to the lateral arm from the summit of the shoulder to the elbow. The purest patch of axillary nerve sensation lies over the lateral portion of the deltoid muscles. This localized sensory area within the C5 dermatome is useful for indicating specific trauma to the axillary nerve, as well as general trauma to the C5 nerve root.
The radial nerve innervates the triceps, extensor carpi radialis and extensor carpi ulnaris, supinator, and extensor pollicis. Motor functions include extension at all arm, wrist, and proximal finger joints below the shoulder; forearm supination; and thumb abduction in the plane of the palm. The triceps is the primary elbow extensor. The radial nerve supplies sensation to the skin over the posterolateral surface of the arm through the posterior brachial cutaneous nerve, posterior antebrachial cutaneous nerve, and the superficial radial nerve branch.
The median nerve innervates flexor carpi radialis, palmaris longus, pronator quadratus, pronator teres, and the digital flexors. Motor functions include thumb flexion and opposition, flexion of digits 2 and 3, wrist flexion and abduction, and forearm pronation. Sensation includes the skin over the anterolateral surface of the hand. When the median nerve is damaged, the thenar eminence may atrophy, and the patient will not be able to oppose the thumb, resulting in an ape-hand deformity.
The ulnar nerve innervates flexor digitorum profundus, adductor pollicis, and small digital muscles. Motor function includes finger adduction and abduction other than the thumb; thumb adduction; flexion of the digits 4 and 5; as well as wrist flexion and wrist adduction. Sensation includes the skin over the medial surface of the hand through the superficial branch. With damage to the ulnar nerve, a
claw-hand deformity is manifested by flattening of the transverse metacarpal arch and longitudinal arches with hyperextension of the metacarpophalangeal (MCP) joints and flexion of the proximal interphalangeal (PIP) and the distal interphalangeal (DIP) joints; these deformities are produced by imbalance of this intrinsic and extrinsic musculature of the fingers.
Summarizing:
- the anterior divisions of the brachial plexus (the musculocutaneous nerve (C5-C6), the median nerve (C6-T1), and the ulnar nerve (C8-T1)) innervate flexor muscles
- the posterior divisions of the brachial plexus (the axillary nerve (C5-C6) and the radial nerve (C5-C8)) innervate extensor muscles.
Reviewing Figure 13.2, a proximal-to-distal gradient is seen for the divisions of the brachial plexus.
Two collateral nerves of the brachial plexus include the long thoracic nerve and the thoracodorsal nerve. Lesions of the long thoracic nerve cause weakness of the serratus anterior muscle, leading to a winged scapula. The thoracodorsal nerve innervates the latissimus dorsi muscle, which adducts, extends, and medially rotates the arm.
Lesions of the brachial plexus include Erb’s palsy, which results in upper arm paralysis caused by injury to the C5-C6 nerve roots. This usually happens during childbirth. It can also result in paralysis of the deltoid, biceps brachii, brachioradialis, supinator, and rotator cuff muscles. Klumpke’s palsy, which is less common, causes paralysis of the intrinsic muscles of the hand by injury of the C8-T1 nerve roots; if the median nerve is involved, an ape hand as well as thenar eminence wasting will be seen. If the ulnar nerve is damaged, a claw hand will be observed.
Damage to the radial nerve has different consequences depending on where the lesion occurs. At the level of the axilla, loss of extensor muscles of the elbow, wrist, and digit will be seen. There will be weakened extension at the shoulder as well as weakened supination. Sensory loss on the posterior arm, forearm, and hand will be seen as well. A pathognomonic sign is wrist drop. Saturday night palsy is caused by compression of the radial nerve against the humerus (such as an intoxicated person in a deep sleep has their arm draped over the back of a chair or couch). This can also be seen with the improper use of crutches. If the lesion occurs in the arm, loss of extensors at the wrist and digits will be seen. Sensory loss on the posterior forearm and hand will occur, but not the posterior arm as the lesion is lower. Wrist drop will also be seen. Fracture of the shaft of the humerus can also lacerate the radial nerve, leading to the same deficits as if the nerve were damaged at the level of the elbow. If a lesion occurs at the level of the wrist, sensory loss on the posterior hand will be observed.
Damage to the median nerve can occur at the level of the elbow or at the level of the wrist. At the level of the elbow, loss of flexion of the digits, thenar muscles, the first two lumbricals, wrist flexion; ulnar deviation upon wrist flexion; and loss of pronation will be apparent. Sensory loss will be on the lateral palm and the first three and a half digits. Seen is an ape hand and flattening of the thenar eminence. At the level of the wrist, loss of function of the thenar muscles and the first two lumbricals is seen. The second and third digit will be “clawed”, and this is referred to as the hand of benediction. Ape hand and flattening of the thenar eminence are again observed. This can occur as a result of carpal tunnel syndrome or wrist laceration.
Damage to the ulnar nerve at the level of the elbow (at the medial epicondyle) will result in weakened wrist flexion, radial deviation upon flexion of the wrist, loss of abduction and adduction of the digits; loss of hypothenar muscles and the third and fourth lumbricals; and weakened flexion of the fourth and fifth digits. Sensory loss will occur on the lateral half of the fourth digit and the fifth digit. A claw hand will be seen. At the level of the wrist, loss of abduction and adduction of the digits is seen as well as loss of the hypothenar muscles and the third and fourth lumbricals. Sensory loss will occur on the lateral half of the fourth digit and the fifth digit A claw hand will again be seen.
Damage to the axillary nerve will cause loss of abduction of the arm in the horizontal plane. This is typically the result of a surgical neck fracture of the humerus or dislocation of the shoulder. Damage to the musculocutaneous nerve is rare; should it occur, loss of elbow flexion and weakness in supination will be present as well as a loss of sensation on the lateral aspect of the forearm.
Thoracic outlet syndrome is caused by compression of the neurovascular structures as they exit through the thoracic outlet and can occur at three possible points. The first narrowing area is the most proximal and is named the interscalene triangle: This triangle is bordered by the anterior scalene muscle anteriorly, the middle scalene muscle posteriorly, and the medial surface of the first rib inferiorly. The presence of the scalene minimus muscle and the fact that both the anterior and middle scalene muscles have their insertion in the first rib can cause a narrow space and therefore compression. The brachial plexus and the subclavian artery pass through this space.
The second area is called the costoclavicular triangle: this is bordered anteriorly by the middle third of the clavicle, posteromedially by the first rib, and posterolaterally by the upper border of the scapula. The subclavian vein, artery and plexus brachialis crosses this costoclavicular region and then further enters the subcoracoid space just distal to the insterscalene triangle. Compression of these structures can occur as a result of congenital abnormalities, trauma to the first rib or clavicle, and structural changes in the subclavian muscle or the costocoracoid ligament.
The third area is called the subcoracoid or subpectoralis minor space: This last passageway is beneath the coracoid process just under the pectoralis minor tendon. The borders of the thoracocoracopectoral space include the coracoid process superiorly, the pec minor anteriorly, and ribs 2-4 posteriorly. Shortening of the pectoralis major can lead to a narrowing of this last space and therefore compression of the neurovascular structures during hyperabduction.
Neurogenic thoracic outlet syndrome is caused by compression of the brachial plexus. Vascular thoracic outlet syndrome is caused by compression of the arteries or veins which pass under the clavicle.
Adson's test is used to assess for the presence of thoracic outlet syndrome. It is performed by compression of the subclavian artery by a tightened anterior or middle scalene. The test is performed with the patient sitting with the elbow in full extension. The arm is then abducted 30 degrees at the shoulder and is maximally extended. The radial pulse is palpated and the physician grasps the patient's wrist. The patient then extends the neck and turns toward the side of the symptomatic shoulder while being asked to take a deep breath and holding it. The quality of the radial pulse is evaluated in comparison to the pulse while the patient's arm is at rest. A positive test is found if there is marked decrease or significant diminishing of the radial pulse. Both sides should be compared.
Neuroanatomy of the lumbosacral plexus
This section was modified from https://accessphysiotherapy.mhmedical.com/data/Multimedia/grandRounds/lumbar/media/lumbar_print.html
The lumbar plexus and the sacral plexus (collectively, the lumbosacral plexus) provide innervation to the lower extremity. (Figure 13.3)
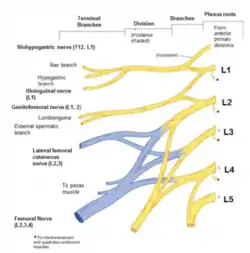 Lumbosacral plexus - lumbar emphasis |
 Lumbosacral plexus - sacral emphasis |
The lumbar plexus is a nervous plexus in the lumbar spine which forms part of the lumbosacral plexus. As with the brachial plexus in the upper extremity, the spinal nerves contributing to the lumbar plexus have both anterior divisions and posterior divisions (anterior divisions are shaded yellow and posterior divisions is shaded blue in the figure above).
The lumbar portion of the plexus is formed by the ventral divisions of the first four lumbar nerves (L1-L4) and also from contributions of the T12 spinal nerve. Additionally, the ventral rami of the L4 spinal nerve passes communicating branches to the sacral plexus. The nerves of the lumbar plexus pass in front of the hip joint and mainly support the anterior portion of the thigh.
The lumbar plexus is formed lateral to the intervertebral foramina and pass through the psoas major muscle. The lumbar plexus’s smaller motor branches are distributed directly to the psoas major, while larger branches leave the muscle at various sites to run obliquely downward through the pelvic area and leave the pelvis under the inguinal ligament (with the exception of the obturator nerve, which exits the pelvis through the obturator foramen).
Consider the functions of the femoral nerve and the obturator nerve in the lower extremity. The femoral nerve gives motor innervation to iliopsoas (which refers to both the psoas and iliacus at their inferior ends), pectineus, sartorius, and the quadriceps muscle group. Motor functions of the femoral nerve include hip flexion at L2-3 ("lift the knee") and knee extension at L3-4 ("kick the door"). The obturator nerve sends motor branches to obturator externus before dividing into an anterior and posterior branch, both of which will continue distally. These branches are separated by adductor brevis and supply all the thigh adductors with motor innervation, including pectineus, adductor longus, adductor brevis, adductor magnus, adductor minimus, and gracilis. The obturator nerve (pictured in darker blue in the figure above) has an anterior branch that supplies the skin on the medial, distal part of the thigh.
The sacral plexus provides motor and sensory nerves for the posterior thigh, most of the lower leg, the entire foot, as well as part of the pelvis. The most clinically important branches arising from the plexus are the sciatic nerve, tibial nerve, and common fibular nerve. Branches from the posterior division are in blue, and branches from the anterior division are in yellow in Figure 13.3. The posterior division leads to the superior gluteal nerve, which innervates the gluteus medius, gluteus minimus, and tensor fasciae latae, whose actions are abducting and medial rotation of the thigh. The inferior gluteal nerve, which innervates the gluteus maximus, acts to extend and laterally rotate the thigh, as well as to extend the lower trunk. The sciatic nerve is the largest peripheral nerve in the body. It is comprised of the tibial and common peroneal nerve and exits the pelvis inferior to the piriformis muscle, between the ischial tuberosity and the greater trochanter of the femur. Motor functions include thigh adduction, medial rotation, and hip extension, as well as knee flexion. The term “sciatica” is a vague term and refers to all disorders causing painful paresthesias in a sciatic distribution.
The tibial nerve is the larger, medial and terminal branch of the sciatic nerve. In the popliteal fossa, it gives off branches to gastrocnemius, popliteus, plantaris, and soleus muscles. The tibial nerve also provides an articular branch to the knee joint and a cutaneous branch that will become the sural nerve. The sural nerve supplies the lateral side of the foot. Below the soleus muscle, the sural nerve lies close to the tibia and supplies tibialis posterior, the flexor digitorum longus, and flexor hallucis longus. The sural nerve passes into the foot running posterior to the medial malleolus; it is bound down by the flexor retinaculum. Motor functions of the tibial nerve include foot plantar flexion and inversion and toe flexion. In the foot, the tibial nerve divides into medial and lateral plantar branches. Cutaneous distribution of the medial plantar nerve is to the medial sole and the medial three-and-a-half toes, including the nail beds on the dorsum (analogous the median nerve in the hand, from the brachial plexus). The lateral plantar nerve cutaneous innervation is to the lateral sole and lateral one-and-a-half toes (analogous to the ulnar nerve which arises from the brachial plexus).
The common fibular nerve divides into the superficial fibular nerve and the deep fibular nerve. The superficial fibular nerve supplies the muscles of the lateral compartment of the leg, including fibularis longus and fibularis brevis. These two muscles help in eversion and plantar flexion of the foot. The deep fibular nerve innervates the muscles of the anterior compartment of the leg, which are tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius. These muscles are responsible for dorsiflexion of the foot and extension of the toes. Clinically, fibular nerve palsy can cause foot drop with weakness of foot dorsiflexion and eversion and sensory loss over the dorsolateral foot and shin. The common fibular nerve supplies sensation to the lateral and anterior surfaces of the upper part of the leg. The superficial fibular nerve supplies sensation to the distal third of the leg and the dorsum of the foot, while the deep peroneal nerve supplies contiguous sides of the first and second toes.