Chapter 5: Clavicle, Sternum, and Ribs
Objectives:
- Describe the bony and cartilaginous articulations of the sternum and clavicle
- Describe the motion of the clavicle during upper limb movement and the sternum during respiration
- Diagnose and treat somatic dysfunctions of the clavicle, sternum, and ribs
- Explain the muscular attachments to the sternum, clavicle, and humerus
- Describe types of motions (caliper/bucket handle/pump handle) seen in the ribs
- Describe gross rib motion in respiration and how the anterior-posterior and lateral diameters of the thoracic cage are affected
- Define typical versus atypical ribs
- Name and describe the articulations of the ribs with the sternum and spinal vertebrae
- Name primary and secondary muscles of respiration, actions and attachments to ribs
Clavicle Anatomy and Somatic Dysfunctions
The function of the clavicle is to connect the upper extremity to the axial skeleton and to extend shoulder range of motion. Clavicle motion is bound by the sternoclavicular joint proximally and the acromioclavicular joint distally. The acromioclavicular (AC) joint is the articulation between the acromion process and the distal clavicle. Its primary motions are abduction as well as internal and external rotation. The sternoclavicular (SC) joint is the articulation between the sternum and the proximal clavicle and it is the only true joint attaching to the upper extremity of the thoracic cage via a saddle-shaped articular surface. Its primary effect is on rib cage motion, as it connects with the manubrium as well as provides ligamentous attachments to the costal cartilage of the ribs. During flexion of the clavicle, the acromial end of the clavicle moves anteriorly; during extension, it moves posteriorly. Somatic dysfunctions have secondary effects on the upper extremity (the glenohumeral joint and the acromioclavicular joint). Motions that occur in the coronal plane include abduction and adduction about an anterior-posterior axis and in the transverse plane include flexion and extension about a superior-inferior axis. Rotation (both internal and external) of the clavicle occurs about a transverse axis in a coronal plane. The costoclavicular ligament connects the clavicle to the first rib and enhances the overall stability. The coracoclavicular ligament prevents displacement of the scapula medially beneath the clavicle.
To assess the clavicle, six ranges of motion should be assessed with the patient in the supine position:
- Clavicle flexion: fold the arm across the chest and utilize the proximal arm to bring the clavicle anteriorly
- Clavicle extension: fold the arm across the chest and utilize the proximal arm to bring the clavicle posteriorly
- Clavicle abduction: the shoulder is shrugged superiorly
- Clavicle adduction: the shoulder is dropped inferiorly
- Clavicle internal rotation: the shoulder is abducted to 90o and rotated forward about the elbow
- Clavicle external rotation: the shoulder is abducted to 90o and rotated backward about the elbow
Clavicular somatic dysfunction is based on reciprocal motion. Rotation of the clavicle occurs along an anterior-posterior axis. Motion of the clavicle is essential for respiration in addition to that of the ribs. First and second rib dysfunctions will often co-exist with clavicular dysfunction.
Somatic dysfunction of the clavicle is named for ease at the distal end (the acromioclavicular end). The clavicle is considered dysfunctional when one paired motion has significantly greater motion when compared to its counterpart (i.e. flexion vs. extension, abduction vs. adduction, internal vs. external rotation). Clavicle somatic dysfunction may involve more than one plane of motion simultaneously. In this case, each component of the somatic dysfunction should be treated individually.
To diagnose clavicle somatic dysfunctions:
- Adducted: the distal end is found to be inferior and resistant to springing along with having poor range of motion. The sternoclavicular joint will be displaced anteriorly and superiorly. (Often coupled with clavicle extension dysfunction.)
- Abducted: the distal end is found to be superior. The clavicle will appear elevated, there will be painful articulation, and restriction and pain at both the AC and SC joints. (Often coupled with clavicle flexion dysfunction.)
- External rotation: the superior ridge of the clavicle will be slightly posterior.
- Internal rotation: the superior ridge of the clavicle will be slightly anterior.
| Example: Clavicle somatic dysfunctions |
|---|
| If the left proximal clavicle is found to be more caudad and posterior on palpation. What is the somatic dysfunction based on these findings? Since the palpatory findings indicate restriction with adduction and extension for the proximal clavicle, and the somatic dysfunction is named for the distal clavicle, the somatic dysfunction is left clavicle abduction and flexion dysfunction. |
As mentioned earlier, the clavicle is involved in scapular and glenohumeral motion. For example, if a patient is found to have a lower right shoulder compared to the left, has trouble extending the right shoulder, and has trouble externally rotating the right shoulder, a clavicle somatic dysfunction can be diagnosed. What is the somatic dysfunction of the clavicle based on these findings? This is a right clavicle adduction, flexion, and internal rotation dysfunction. This somatic dysfunction can be treated with muscle energy by placing the patient in the restrictive barrier and using post-isometric relaxation.
| Example: Clavicle somatic dysfunction treatment with post-isometric muscle energy |
|---|
| How would a clavicular adduction dysfunction be treated utilizing post-isometric muscle energy? By shrugging the shoulders for 3-5 seconds against resistance 3-5 times. |
In the absence of any other dysfunction, a shoulder height discrepancy can also be explained by an ipsilateral hypertonic trapezius muscle which will cause elevation of the scapula and may not necessarily be attributed to a clavicular dysfunction.
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Trapezius muscle |
|
|
|
CN XI, cervical plexus (C2-C4) | 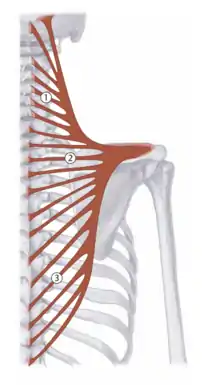 Trapezius: 1 - descending; 2 - transverse; 3 - ascending |
Treatment of clavicle somatic dysfunctions with post-isometric muscle energy techniques:
| Clavicle flexion dysfunction | Patient is supine and towards the edge of the table. Contact the dysfunctional clavicle towards the distal end. Extend the clavicle to the restrictive barrier, taking care to stabilize the patient. Ask patient to flex their clavicle, and meet the patient force to create an isometric contraction. After 3-5 seconds, have patient relax, and reposition the clavicle to its new restrictive barrier. | 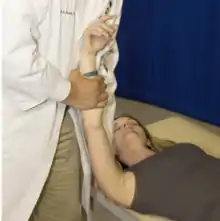 Clavicle flexion somatic dysfunction treatment |
|---|---|---|
| Clavicle extension dysfunction | Patient is supine. Contact the dysfunctional clavicle towards the distal end. Flex the clavicle to the restrictive barrier, taking care to stabilize the patient. May use the upper extremity as a lever. Ask patient to extend their clavicle, and meet the patient force to create an isometric contraction. After 3-5 seconds, have patient relax, and reposition the clavicle to its new restrictive barrier. | 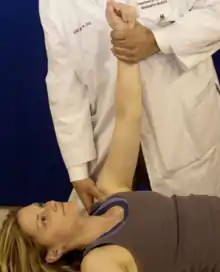 Clavicle extension somatic dysfunction treatment |
| Clavicle abduction dysfunction | Patient is supine. Contact the dysfunctional clavicle towards the distal end. Adduct the clavicle to the restrictive barrier, taking care to stabilize the patient. May use the upper extremity as a lever. Ask patient to abduct their clavicle, and meet the patient force to create an isometric contraction. After 3-5 seconds, have patient relax, and reposition the clavicle to its new restrictive barrier. |  Clavicle abduction somatic dysfunction treatment |
| Clavicle adduction dysfunction | Patient is supine. Contact the dysfunctional clavicle towards the distal end. Abduct the clavicle to the restrictive barrier, taking care to stabilize the patient. May use the upper extremity as a lever. Ask patient to adduct their clavicle, and meet the patient force to create an isometric contraction. After 3-5 seconds, have patient relax, and reposition the clavicle to its new restrictive barrier. |  Clavicle adduction somatic dysfunction treatment |
| Clavicle internal rotation dysfunction | Patient is supine. Abduct dysfunctional shoulder to 90 degrees. Contact the dysfunctional clavicle towards the distal end. Externally rotate the upper extremity until the clavicle externally rotates to the restrictive barrier, taking care to stabilize the shoulder. Ask patient to internally rotate their upper extremity, and meet the patient force to create an isometric con traction. After 3-5 seconds, have patient relax, and reposition the upper extremity to its new restrictive barrier. |  Clavice internal rotation somatic dysfunction treatment |
| Clavicle external rotation dysfunction | Patient is supine. Abduct dysfunctional shoulder to 90 degrees. Contact the dysfunctional clavicle towards the distal end. Internally rotate the upper extremity until the clavicle internally rotates to the restrictive barrier, taking care to stabilize the shoulder. Ask patient to externally rotate their upper extremity, and meet the patient force to create an isometric contraction. After 3-5 seconds, have patient relax, and reposition the upper extremity to its new restrictive barrier. |  Clavicle external rotation dysfunction treatment |
Sternum Anatomy and Somatic Dysfunctions
The sternum has three parts:
- the head, or manubrium
- the body, or gladiolus;
- the tail, or xiphoid process.
The angle of Louis is the site of the second rib attachment. Upon deep inhalation, the entire sternum glides superiorly, and the inferior end moves anterior. Upon exhalation, the entire sternum glides inferiorly, and the inferior end moves posteriorly. Motion at the sternal angle allows for anterior and posterior motion.
Motion occurs at the sternum in four planes:
- flexion/extension (about a transverse axis)
- rotation (about a vertical axis)
- sidebending (about an anterior-posterior axis)
- superior/inferior glide of the entire sternum
Assessing the manubrium: To assess flexion/extension, place one thumb on the superior border of the manubrium and place the other thumb just above the angle of Louis. Assess springing motion. To assess sidebending, place fingers on superior and inferior lateral borders on opposite sides of manubrium springing medially. To assess rotation, place thumb on each lateral border of the manubrium. Assess spring.
Assessing the gladiolus: To assess flexion/extension, place one thumb just below the angle of Louis and place other thumb on inferior border of gladiolus just above the xiphoid process. Assess springing. To assess sidebending, place thumb on each lateral border of the gladiolus. Spring. To assess rotation, place fingers on superior and inferior lateral borders on opposite sides of gladiolus. Spring medially.
To assess the sternum, place one thumb on superior border of manubrium, other on angle of Louis. Spring. If the superior border springs better, this is an extension somatic dysfunction of the manubrium. If the inferior border springs better, this is a flexion somatic dysfunction of the manubrium. Repeat this test on superior and inferior borders of body of gladiolus. Next, check the angle of the sternum for side bending preference. Spring the lateral margins to assess rotational somatic dysfunction. Last, move the entire sternum in circular motion; check for “drag” in the superior, inferior, and lateral directions. Do not spring the xiphoid! To name somatic dysfunction of the sternum, use the same principles used to name vertebral somatic dysfunction; somatic dysfunction is named by the movement of an imaginary dot on the anterosuperior surface of the bone of reference and named for the preferred direction of motion. Somatic dysfunction of the gladiolus, if present, will usually be opposite of manubrium.
| Example: Sternum somatic dysfunction diagnosis and treatment |
|---|
|
1. If a patient presents following an altercation with a prominent sternal angle and demonstrates a lack of spring when palpating just inferior to the angle of the sternal body, with no other restrictions appreciable in either sidebending or rotation, the somatic dysfunctions associated with the manubrium and the gladiolus are extension dysfunction of the manubrium and flexion dysfunction of the gladiolus.
|
Ribs Anatomy and Somatic Dysfunctions
The ribs can be classified as true ribs, false ribs, and floating ribs. The true ribs are ribs 1-7 and named as such because they attach to the sternum. The false ribs are ribs 8-10 which are attached via cartilage to each other and then to the cartilage of rib 7 and the floating ribs. The floating ribs are ribs 11 and 12, which do not connect to either cartilage or the sternum. The lowest rib attachment connects superiorly to the xiphoid process (rib 10 through costal cartilage).
The typical ribs include ribs 3-9. Present on the typical ribs is the knob-like rib head, the rib neck, the tubercle, the rib body, the angle of the rib, and the costal groove. Each typical rib has two facets which form costovertebral articulations. One articulates with the vertebral body above and the other with the vertebral body at the same level. A third facet, at the tubercle, articulates with the transverse process of the vertebra at the same level forming the costotransverse articulation. For example, rib 3 would articulate with T2 (inferior facet) and T3 (superior facet). The costochondral articulations connect the ribs to the costal cartilage, and the sternochondral articulations connect the costal cartilage to the sternum (without direct connection to the ribs).
The atypical ribs are ribs 1, 2, 10, 11, and 12:
- Rib 1 is flat, has the greatest curvature, the shortest length, no angle, no costal groove, and has one facet at its rib head that articulates only with the body of T1
- Rib 2 is similar to rib 1 but it is longer and not as flat. It has two demifacets on its rib head that articulate with the body of T1 and T2.
- Rib 10 is similar in structure to the typical ribs except that it only has one facet on the rib head which articulates with the body of T10.
- Ribs 11 and 12 have no neck, no tubercles, and only one facet on the rib head articulating with the corresponding vertebral body.
Rib motion is influenced by the angle between the vertebral body and the transverse process as well as the distance between the costal articulations with the vertebrae. Rib motion is characterized by one of three motions. Pump handle (ribs 1-5) motion describes motion like an old-fashioned water pump that during inhalation increase the anterior-posterior diameter. Bucket handle motion (ribs 6-10) describes motion where both ends are fixed, and the transverse diameter increases with inhalation. Mixed pump handle and bucket handle motions occur from ribs 1-10, but the primary motion is as described above. Caliper motion (ribs 11 and 12) occurs when both anterior/posterior and transverse dimensions change with respiratory cycles; these ribs do not have connections with the sternum. Movement is like calipers opening and closing.
Muscles involved in the respiratory cycle are listed below:
| Muscles of inspiration |
+ used for treatment of inhalation dysfunctions with respiratory-assisted muscle energy |
|---|---|
| Accessory muscles of inspiration |
++ used for treatment of exhalation dysfunctions with respiratory-assisted muscle energy |
| Muscles of exhalation |
|
Rib somatic dysfunctions may cause chest, back, shoulder, arm, or neck pain; they may be primary dysfunctions but always accompany a thoracic dysfunction. Always treat thoracic dysfunctions prior to treating any rib dysfunctions. Rib somatic dysfunctions may be classified as an exhalation dysfunction or an inhalation dysfunction. Both exhalation and inhalation dysfunctions typically affect a group of ribs.
Exhalation dysfunctions (i.e. inhalation restrictions; “stuck down”) may be treated with muscle energy using the key rib, which is the most cephalad (the “top”) rib. Using respiratory effort and accessory muscles of inhalation, muscle energy techniques can be used to treat these dysfunctions.
For treating inhalation dysfunctions, the key rib is the most caudad (the “bottom”) rib. Using respiratory effort and the muscles of exhalation, muscle energy techniques can be used to treat these dysfunctions. The quadratus lumborum muscle is used to treat exhalation dysfunctions of ribs 11-12. The latissimus dorsi is the “cough” muscle; dysfunctions from acute illness which have a large amount of coughing can have rib dysfunctions associated with this muscle.
| Origin | Insertion | Action | Innervation | Schematic (from Thieme) | |
|---|---|---|---|---|---|
| Respiratory diaphragm: |
|
Central tendon | Respiration | Phrenic nerve (C3-C5) | 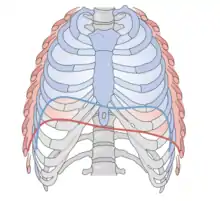 Diaphragm: red - inhalation; blue - exhalation |
| Scalene muscles (anterior, middle, and posterior): |
|
|
|
Cervical plexus and brachial plexus (C3-C6) | 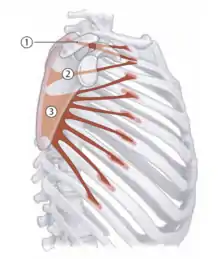 Serratus anterior |
| Pectoralis minor | Ribs 3-9 | Coracoid process | Scapular retraction; respiration | Medial and lateral pectoral nerves (C6-T1) |  2 - Pectoralis minor |
| Serratus anterior | Ribs 1-9 | Scapula | Draw scapula laterally forward (protraction); respiration | Long thoracic nerve (C5-C7) | 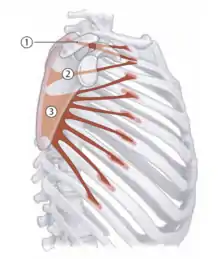 Serratus anterior |
| Latissimus dorsi |
|
Lesser tuberosity of the humerus |
|
Thoracodorsal nerve (C6-C8) | 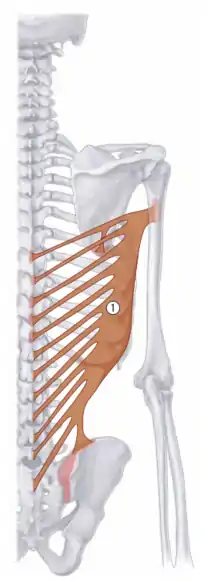 1 - Latissimus dorsi |
| Quadratus lumborum | Iliac crest | Rib 12; L1-L4 |
|
Subcostal (12th intercostal) nerve | 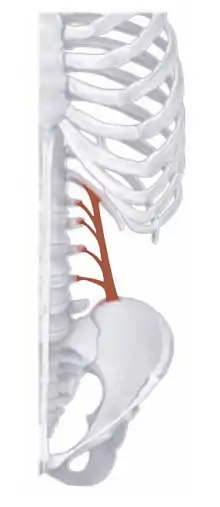 Quadratus lumborum |
Respiratory-assisted muscle energy treatments of rib somatic dysfunctions:
| Inhalation dysfunction key ribs 1-10 (respiratory diaphragm) | Patient is supine. Physician sits/stands either at the head of the table or to the side of the table. Contact the lateral portion of the key rib with firm pressure, using as broad contact as possible. Be sure to avoid any sensitive areas (i.e. breast tissue). Apply a caudad force on the key rib, exerting just enough pressure to feel tension over the dysfunctional ribs. Supporting the patient’s head and upper body, sidebend the patient to the same side as the key rib, using the key rib as a fulcrum. Ask the patient to perform a cycle of forced maximal inhalation and exhalation. During the exhalation phase, increase caudad pressure on the key rib and sidebending around the key rib. |  Upper ribs inhalation dysfunction  Lower ribs inhalation dysfunction |
|---|---|---|
| Inhalation dysfunction key ribs 11-12 (respiratory diaphragm) | Patient is prone. Physician is standing on the side of the table opposite the key rib. Contact the key rib with firm anterior pressure over the lateral edge of the rib. Ask the patient to perform a cycle of forced max- imal inhalation and exhalation. During the exhalation phase, increase anterior/medial pressure on the lateral edge of the key rib. | 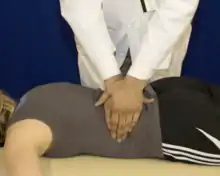 Ribs 11-12 inhalation dysfunction |
| Exhalation dysfunction key rib 1 (anterior/middle scalenes) | Patient is supine. Ask patient to place the dorsum of their dysfunction-side hand on their forehead. Contact the key rib as close to the costotransverse junction as possible with one hand, and stabilize the patient’s head/hand with the other hand. Ask the patient to perform a forced maximal inhalation and simultaneously try to lift their head off the table. Resist their head motion, and during the inhalation phase apply a caudad force on the key rib at the costotransverse junction. |  Rib 1 exhalation dysfunction |
| Exhalation dysfunction key rib 2 (posterior scalene) | Patient is supine. Ask patient to place the dorsum of their dysfunction-side hand on their forehead, and then rotate their head away from the side of the key rib. Contact the key rib as close to the costotransverse junction as possible with one hand, and stabilize the patient’s head/hand with the other hand. Ask the patient to perform a forced maximal inhalation and simultaneously try to lift their head off the table. Resist their head motion, and during the inhalation phase apply a caudad force on the key rib at the costotransverse junction. | 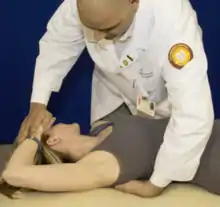 Rib 2 exhalation dysfunction |
| Exhalation dysfunction key ribs 3-5 (pectoralis minor) | Patient is supine. Ask the patient to place their dysfunction-side arm in abduction to 90 degrees. The elbow may be flexed to allow for better positioning. Contact the key rib as close the costotransverse junction as possible with one hand, and stabilize the patient’s elbow with the other hand. Ask the patient to perform a forced maximal inhalation and simultaneously try to lift their elbow straight off the table. Resist their elbow motion, and during the inha- lation phase apply a caudad force on the key rib at the costotransverse junction. |  Ribs 3-5 exhalation dysfunction |
| Exhalation dysfunction key ribs 6-8 (serratus anterior) | Patient is supine. Ask the patient to place their dysfunction-side arm in abduction to 90 degrees. The elbow may be flexed to allow for better positioning. Contact the key rib as close the costotransverse junction as possible with one hand, and stabilize the patient’s elbow with the other hand. Ask the patient to perform a forced maximal inhalation and simultaneously try to bring their elbow across their body towards the contralateral ASIS. Resist their elbow motion, and during the inhalation phase apply a caudad force on the key rib at the costotransverse junction. |  Ribs 6-8 exhalation dysfunction |
| Exhalation dysfunction key ribs 9-10 (latissimus dorsi) | Patient is supine. Ask the patient to place their dysfunction-side arm in abduction to 90 degrees. The elbow may be flexed to allow for better positioning. Contact the key rib as close the costotransverse junction as possible with one hand, and stabilize the patient’s elbow with the other hand. Ask the patient to perform a forced maximal inhalation and simultaneously try to adduct their elbow. Resist their elbow motion, and during the inhalation phase apply a caudad force on the key rib at the costotransverse junction. |  Ribs 9-10 exhalation dysfunction |
| Exhalation dysfunction key ribs 11-12 (quadratus lumborum) | Patient is prone. Physician is standing on the side of the table opposite the key rib. Contact the key rib with firm anterior pressure over the costotransverse junction of rib with one hand, and hold onto the ASIS on the dysfunctional side with the other hand. Ask the patient to perform a cycle of forced maximal inhalation and exhalation. During the inhalation phase, increase anterior/lateral pressure on the costotransverse junction of the key rib, while pulling posteriorly slightly on the ASIS to stabilize the pelvis. |  Ribs 11-12 exhalation dysfunction |
Anterior rib tenderpoints are associated with exhalation dysfunctions. Posterior rib tenderpoints are associated with inhalation dysfunctions and are associated with spasm of the levatores costarum muscle. Rib dysfunctions can also be treated with counterstrain.
| Rib counterstrain tenderpoints |
|---|
 Rib counterstrain tenderpoints |
Reference: 1. Nicholas AS, Nicholas EA. Atlas of Osteopathic Techniques. Philadelphia, PA: Lippincott Williams and Wilkins, 2016. Page 179.
| Tenderpoint | Location | Acronym |
|---|---|---|
| AR1 | Below clavicle at first chondrosternal articulation | Supine, F STRT |
| AR2 | On second rib at midclavicular line | Supine, F, STRT |
| AR3-AR10 | Anterior axillary line on dysfunctional rib | Seated, F STRT |
| PR1 | Cervicothoracic angle just anterior to trapezius | Seated, E, SART |
| PR2-PR10 | Superior surface of respective rib angles | Seated, F SARA |
Review Questions
1. Which of the following appropriately characterizes extension of the clavicle?
A. The acromial end of the clavicle moves anteriorly
B. The acromial end of the clavicle moves posteriorly
C. The sternal end of the clavicle moves inferiorly
D. The sternal end of the clavicle moves superiorly
2. A patient is examined and found to have a sternoclavicular joint that glides inferiorly on the left with shoulder shrug and has no appreciable motion on the right. What is the somatic dysfunction diagnosis?
A. Right clavicle adducted
B. Left clavicle adducted
C. Right clavicle abducted
D. Left clavicle abducted
3. A patient presents with the findings that demonstrate the left proximal clavicle is more caudad and posterior. What is the somatic dysfunction diagnosis?
A. Left clavicular abduction and extension dysfunction
B. Left clavicular abduction and flexion dysfunction
C. Left clavicular adduction and extension dysfunction
D. Left clavicular adduction and flexion dysfunction
4. A patient is found to have a lower right shoulder compared to the left, has trouble extending the right shoulder, and has trouble externally rotating the right shoulder. A clavicle somatic dysfunction can be diagnosed. What is the somatic dysfunction of the clavicle based on these findings?
A. Right clavicle abduction, flexion, external rotation dysfunction
B. Right clavicle adduction, flexion, internal rotation dysfunction
C. Right clavicle adduction, extension, internal rotation dysfunction
D. Right clavicle abduction, extension, external rotation dysfunction
E. Right clavicle abduction, flexion, internal rotation dysfunction
5. A patient is diagnosed with a left clavicle adduction, extension, and internal rotation dysfunction. Which of the following is true regarding utilizing post-isometric muscle energy techniques to treat somatic dysfunctions of the clavicle?
A. The somatic dysfunctions in each respective plane of motion should be treated all at once.
B. The somatic dysfunctions in each respective plane of motion should be treated individually.
C. Lower extremity somatic dysfunctions should be addressed prior to addressing clavicle somatic dysfunctions.
D. Post-isometric muscle energy is not an appropriate technique to address this somatic dysfunction.
6. Which of the following statements is true regarding the atypical ribs?
A. Rib 10 is flat, has the greatest curvature, the shortest length, no angle, no costal groove, and has one facet at its rib head that articulates only with the body of T1
B. Rib 2 is similar to rib 1 but it is longer and not as flat. It has two demifacets on its rib head that articulate with the body of T1 and T2
C. Rib 2 is similar in structure to the typical ribs except that it has only one facet on the rib head which articulates with the body of T10
D. Ribs 11 and 12 have no neck, no tubercles, and only one facet on the rib head articulating with the corresponding vertebral body
Questions 7-11: Match the following descriptions with the listed treatment technique.
7. Ribs 1-2
8. Ribs 3-5
9. Ribs 6-9
10. Ribs 9-10
11. Ribs 11-12
A. Anterior and middle scalenes
B. Serratus anterior
C. Quadratus lumborum
D. Pectoralis minor
E. Latissimus dorsi
12. Consider a right ribs 3-6 exhalation dysfunction. What is the key rib in treating this dysfunction with muscle energy and what is the primary motion of these ribs?
A. Rib 3; Pump handle
B. Rib 3; Bucket handle
C. Rib 3; Caliper
D. Rib 6; Pump handle
E. Rib 6; Bucket handle
F. Rib 6; Caliper
13. To which of the following structures does rib 4 articulate?
A. T2, T3, and T4
B. T3 and T4
C. T3 only
D. T4 only
E. T4 and T5
14. Which of the following correctly describes sternal motion during a respiratory cycle?
A. Upon deep inhalation, the entire sternum glides inferiorly.
B. Upon deep inhalation, the inferior end of the sternum moves anteriorly.
C. Upon exhalation, the entire sternum glides superiorly.
D. Upon exhalation, the inferior end of the sternum moves caudad.
15. A 30-year-old female presents for follow up of reactive airway disease. She notes that her asthma has been well controlled with inhaled corticosteroids. She notes a recent asthma attack in the last week during which she has had residual left-sided rib pain. Vital signs are stable. On physical exam, her breath sounds are clear to auscultation bilaterally without rales, wheezing, rhonchi, or accessory muscle use. Muscle strength testing, deep tendon reflexes, and sensation testing are unremarkable. T3-T6 are noted to have paraspinal hypertonicity on the right. Ribs 3-6 are noted to be stuck down on the left. She has restriction of the right hemidiaphragm. Which of the following is accurate with regard to this rib dysfunction?
A. Binding or immobilization of the ribs is recommended to improve rib pain.
B. Thoracic spine somatic dysfunctions should be treated prior to treating the ribs.
C. The affected ribs are atypical ribs.
D. The affected ribs are false ribs.
E. Muscle energy techniques are contraindicated in this patient.
16. Which of the following statements regarding somatic dysfunctions of the ribs is correct?
A. Anterior rib tenderpoints are associated with spasm of the levatores costarum muscle.
B. Anterior rib tenderpoints are associated with ribs that prefer to remain cephalad.
C. Posterior rib tenderpoints are associated with inhalation dysfunctions.
D. Dysfunctional ribs 1-6 will show a bucket handle motion.
E. The initial setup for a counterstrain treatment of a posterior rib dysfunction Is with the patient supine, extended, sidebent toward the tenderpoint, and rotated away.
Answers to Review Questions
- B
- A
- B
- B
- B
- D
- A
- D
- B
- E
- C
- A
- B
- B
- B
- C