Chapter 14: Osteopathic Cranial Manipulative Medicine
Objectives:
- Describe the structure, relative positions, articulations, and mutual attachments for the cranial bones, cranial membranes, cranial venous sinuses, and the foramen and location of the cranial nerves
- Define the Primary Respiratory Mechanism (PRM) and its normal phases
- Define the Core Link and its attachments
- Identify and describe the five principles of the primary respiratory mechanism
- Define the axes and relative motions of the following cranial somatic dysfunctions: flexion, extension, torsion, sidebending-rotation, lateral strain, vertical strain, and compression
Introduction to Osteopathic Cranial Manipulative Medicine
Osteopathic Cranial Manipulative Medicine was pioneered by William Sutherland, DO after he saw a disarticulated skull and noted that bevels in the joints’ changes (i.e. the squama) resembled the gills of a fish which indicated articular mobility for a respiratory mechanism. Dr. Sutherland found out by experimenting on himself that manipulation could bring about a range of reactions that varied from physiological to emotional changes. Sutherland concluded that good physical and mental health depends not only one the bones of the skull being in the right position, but also on the ability of the sutures to allow for slight movement. Sutherland, after thirty years of research on this self-regulating movement, identified what he termed the primary respiratory mechanisms (PRM) or the cranial rhythmic impulse (CRI). This mechanism is characterized by light movement of the bones in the skull and sacrum, the membrane system (visceral) and the central nervous system cerebrospinal fluid.
The 5 principles of the primary respiratory mechanism include:
- Inherent motility of the brain and spinal cord
- Fluctuation of cerebrospinal fluid
- Motility of membranes
- Articular mobility of the cranial bones
- Involuntary mobility of the sacrum between the ilia
Motility refers to inherent movement; mobility refers to free movement.
Inherent motility of the brain and spinal cord is a subtle, slow, rhythmic movement with biphasic cycle (flexion and extension). This rhythmic activity has a range of 10-14 cycles/minute. Physiologic centers controlling respiration, circulation, digestion, and elimination are located in the floor of the 4th ventricle and depend on the proper functioning of the CNS. Studies from radiology and neurology have demonstrated the validity of the PRM phenomenon. Evidence suggests that neuroglial cells of the CNS move rhythmically, in unison, resulting in the biphasic cycle of the PRM. This contraction around the lateral ventricles is the motion that is responsible for the remaining 4 principles of the PRM.
Fluctuation of cerebrospinal fluid (abbreviated CSF) involves a “wave-like” motion of the fluid which circulates and bathes the brain and spinal cord. The biphasic rhythm of the CNS changes the shape of the ventricles, propelling the CSF forward. The combined actions of CNS motility and CSF fluctuation manifest as bioelectric activity throughout the body and can be palpated at any point on the body. Cerebrospinal fluid (CSF) is produced by both choroid plexuses - structures lining the floor of the two lateral ventricles and the roof of the third and fourth ventricles; a ventricle is an interior fluid space of the brain - and weeping of tissue fluid by the brain into the ventricles. Once produced, the CSF circulates from these ventricles to the subarachnoid fluid space (a fluid space investing the brain and spinal cord) outside the brain. The CSF then reaches structures (arachnoid villi) along the superior, midline surface of the brain where it is reabsorbed back into the blood vessels (sagittal sinus).
Motility of membranes involves the dura mater and its attachments to the skull. The dura mater has two layers: the outer layer is continuous with the inner table of the cranial cavity, continuous through the sutures to become the periosteum of the outer table of the skull. The inner layer of the dura covers the brain and spinal cord and has reduplications named the falx cerebri and tentorum cerebelli, which invest in the various bones of the cranium. The falx cerebri and tentorum cerebelli will be discussed in more detail later.
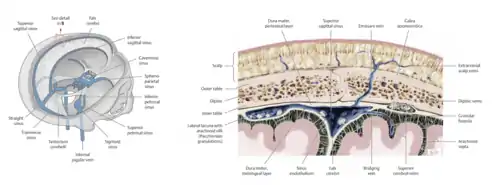
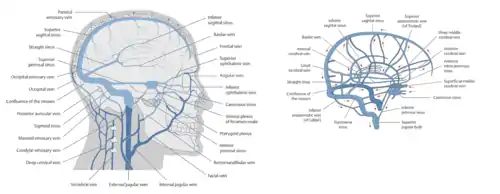
The 2 layers of the dura are fused in some areas and separated in others, forming the intradural venous sinuses. Notable structures of the venous sinuses include the superior sagittal sinus, the inferior sagittal sinus, the straight sinus, the transverse sinus, the confluence of sinuses, and the occipital sinus.
The dura mater has firm attachments to the foramen magnum, and the C2, C3, and S2 spinal segments. The dura mater is innervated by the trigeminal nerve: CN V1 innervates the anterior fossa, CN V2 innervates the middle cranial fossa, and CN V3 innervates the greater wing of the sphenoid and the mastoid air cells. The spinal nerves of C1 and C2 innervate the posterior cranial fossa.
The falx cerebri arises from the straight sinus and attaches to the occiput to the internal occipital protuberance, the parietal bones at the borders of the sagittal sinus, the frontal bone at the borders of the sagittal sinus, and the ethmoid bone at the crista galli. The two halves of the tentorium cerebelli arise at the straight sinus and attach to the occiput, temporal, and sphenoid bones. The tentorum cerebelli forms the room of the cavernous sinus, contains CN III, CN IV, CN V1, CN VI, and the internal carotid artery as well as encapsulates the pituitary gland.
The attachments to the dura mater, as mentioned previously, are the foramen magnum in addition to the C2, C3, and S2 spinal segments. The articular surfaces of the sacrum have voluntary movement on one of several postural axes in relation to the ilia. There is involuntary mobility of the sacrum between the ilia as a result of the inherent motility of the CNS, fluctuation of the CSF, and the pull of the membranes. Sacral motion is palpated as a slight rocking motion at the respiratory axis, at the level of S2.
The primary respiratory mechanism is characterized by elevation of the third ventricle which elevates the pituitary and moves the sella turcica cephalad, the anterior movement of the tentorum cerebelli during which the clinoid process shifts superiorly and posteriorly (affecting the sphenoid bone) and the attachments to the petrous ridge move superiorly and anterolaterally (affecting the temporal bones). This biphasic cycle influences movement of the bones of the cranium and the sacrum via their attachments, collectively referred to as the Core Link and is palpated as the synchronous, involuntary movement of the occiput and the sacrum. The unit involving the dura and the attachments is named the reciprocal tension membrane. These membranes respond to motion of the CNS and the fluctuation of the CSF. This synchronous motion of the occiput and sacrum is influenced by the rhythmic pull of the spinal and cranial dura mater attached between them; it transmits forces by linking the cranium to the sacrum.
Traumas and postural strains affecting part of the reciprocal tension membrane affect function of the entire unit. At birth, the bones have smooth edges. During development of the skull, the bones of the cranial base that are pre-formed in cartilage are the occiput (except for the upper squama); the pteromastoid part of the temporal bones; the body, the lesser wings, and the roots of the greater wings of the sphenoid bone; and the ethmoid bone. The articular mobility of the cranial bones occurs during development when they interdigitate with the movement of the CNS. With growth and motion, the edges develop sutures between them which allows for a minimal amount of motion as well as provides protection for the brain. This movement contributes to a homeostatic mechanism known as cranial compliance. The cranial vault or calvarium (membranous) is made of curved plates of mesenchyme at the side of the skull that extend cranially to blend with each other; they also extend toward the base of the skull. Once the sutures are formed and mineralized bone exists, there is a second phase in which growth of cranial bones occurs at the sutural margins. These dermal bones are the frontal bones, the parietal bones, the squamous parts of the temporal bones, and the upper occipital squama.
Anatomy of the Head (Cranium)
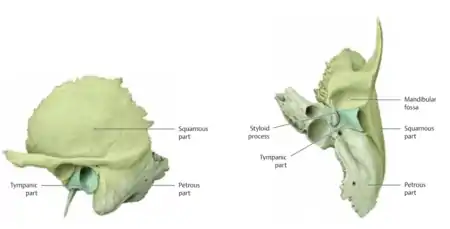
Anatomic landmarks in the skull which should be identified include the frontal bone, the parietal bone, the temporal bone (including the squamous portion, the petrous portion, and the tympanic portions), the sphenoid bone (including the greater wing and the lesser wing), the occipital bone, the zygomatic bone (or zygoma), the maxilla bone, the mandible bone, the ethmoid bone, the lacrimal bone, and the nasal bone.
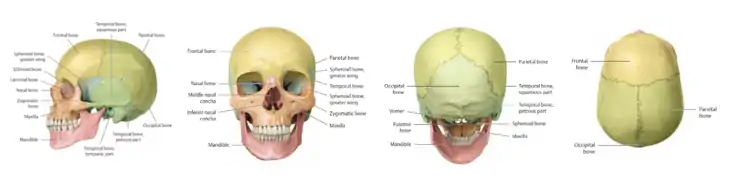
It is useful to be able to identify the structures on your own face in addition to a model (such as a disarticulated skull) as well. As with the axial and appendicular spine, landmarks are critically important for palpation. If you were to palpate above your ears and clench your teeth, the muscle being contracted is the temporalis muscle, which attaches to the temporal bone. The parietal bone is superior and posterior to the temporal bone. The zygomatic process of the temporal bone articulates with the zygomatic bone. What a lay person considers to be the “cheek bone” is made up of the zygomatic bone on the anterior surface and the projection of bone which can be felt with a pincer grip moving posteriorly is the zygomatic process of the temporal bone. Posterior to the ear is the mastoid process. Patients may present with a complaint of ear pain which is often mistakenly initially assumed to be due to otitis media but is more likely a temporomandibular joint dysfunction or dysfunctions involving the muscles which attach to the mastoid process. An unremarkable ear examination is a likely indicator that otitis media is not the origin of the patient’s symptoms. The junction of sutures of the frontal bone and both parietal bones is known as bregma; the junction of sutures of the occiput and both parietals is known as lambda
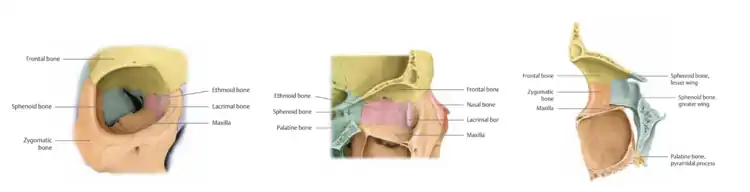
The orbit is made up of several bones: the frontal bone, the maxilla, the zygomatic bone, the sphenoid bone, the lacrimal bone, and the ethmoid bone.
The flat portion of the temporal bone is the squamous portion. The zygomatic process helps to comprise the zygomatic arch. Through the space on the temporal bone is where the temporalis muscle traverses. The mastoid process is a conical prominence of the temporal bone behind the ear, to which neck muscles including the sternocleidomastoid muscle are attached, and which has air spaces linked to the middle ear. The styloid process is the site of attachment of the stylohyoid muscle as well as strands of the tongue. The serrated, jagged edge of the temporal bone on the inner portion of squamous portion contains bevels which Sutherland described as having motions similar to the gills of a fish.
The portion of the temporal bone that runs horizontally and flatly is the petrous part of the temporal bone; the edge of the petrous portion is the petrous ridge. The external auditory meatus can also be identified. The indentation on the inner side of the temporal bone is what forms the boundary of the transverse sinus becoming the sigmoid sinus just prior to exiting the head. The petrous ridge, embryologically, forms because of the tension from the tentorum cerebelli. Moreover, the pull of the dura on the bone leads to indentations resembling lines as it develops and also serves to create the landmarks. The cerebellar fossa is just inferior to the location of the cerebral hemispheres.
A particularly important landmark is the foramen magnum; it is located at the base of the occiput. The coronal section through the sinuses shows the crista galli of the ethmoid bone, the frontal sinus, the superior nasal concha, the middle nasal concha, the inferior nasal concha, the orbit, the maxillary sinus, and the vomer.

Figure 14.6 - Formamen Magnum
View the cranium as a system of cogwheels and pulleys. The brain has its motility changing the ventricles shape, exerting an external force in the membranes, sinuses and indirectly the cranial bones. The membranes have their own motility which exerts a force on the brain, the venous sinuses, the cranial bones and the sacrum. The CSF production and absorption exerts a force on the ventricles/brain, membranes and cranial bones. There is a collective orchestration of motion. Start to view the cranium as an integral part of the body that has motion within itself and how these motions have biomechanical effects locally and distally. These cogwheels and pulleys affect hormonal production and nerve conduction. Don’t get stuck on what are the motions but rather what are the structures involved.
The sphenobasilar synchondrosis (SBS) is a major anatomic consideration in osteopathic cranial manipulative medicine. It is an articulation of the sphenoid with the occiput. It is the keystone of all cranial movement. Two motions that occur at the SBS are flexion and extension. There are two types of bones involved with the PRM: the paired bones, which consist of the parietal bones and the temporal bones, and the midline (or single) bones, which consist of the sphenoid bone, the occiput bone, the vomer, and the sacrum. Motions occur on the order of the 1-2 mm range but are structurally significant. The greater wing of the sphenoid bone is just behind the eye and can be palpated on your own face. Feel the ridge of the lateral eye and move just behind it to palpate the greater wing of the sphenoid bone.
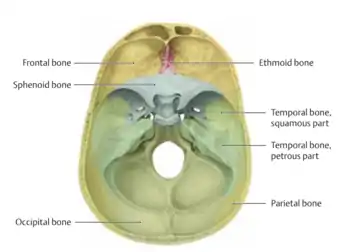
The jugular foramen, through which the vagus nerve exits, is formed by the junction of the temporal and the occipital bones. The sella turcica is where the pituitary gland sits. The clinoid processes are portions of the sphenoid bone which are a boundary of the sella turcica. Flat ridges of the cranial bones are dural attachments; if the flat ridges occur in a horizontal plane this is as a result of tension from the tentorium cerebelli and if the flat ridges occur in a vertical plane it is from tension of the falx cerebri. The bevels of the temporal bones change orientation: at the top portion the bevel is facing inward and at the bottom portion the bevel is facing outward. The bevel crosses and switches sides suggesting a hinge motion and is indicative of a rotational component.
During flexion, the midline bones of the cranium (sphenoid, occiput, ethmoid, and vomer) move through a flexion phase. The paired bones of the cranial move through external rotation phase. Flexion at the SBS causes the dura to be pulled cephalad, moving the sacral base posterior through the superior transverse axis (at the level of S2) of the sacrum, which is known as counternutation, also known as sacral extension. Flexion will widen the head and slightly decrease the anteroposterior diameter.
During extension, the midline bones of the cranium (sphenoid, occiput, ethmoid, and vomer) move through an extension phase. The paired bones of the cranial move through an internal rotation phase. Extension at the SBS causes the dura to fall caudad, moving the sacral base anterior through the superior transverse axis (at the level of S2) of the sacrum, which is known as nutation, also known as sacral flexion. Extension will narrow the head and slightly increase the anteroposterior diameter.
Cranial Somatic Dysfunctions
Particular indications for craniosacral treatment include atypical facial pain, headaches, sinusitis, otitis media, tinnitus, vertigo, temporomandibular joint dysfunction, plagiocephaly, and childbirth, among others.
Palpation of the PRM is very subtle. At first, the physician may be palpating thoracic respirations – if so, ask the patient to hold their breath. With experience and practice, physicians can learn to filter out respiration and focus on the primary respiratory mechanism. The physician should sit with forearms resting on the table, find a relaxed position, have no tension in your arms, and gently let your palms and fingers conform to your partner’s head while keeping thumbs off the head. The touch is gentle, not crushing; light but not as a feather. There must have been definite contact; optimum placement and contact takes practice. The physician’s mind must be quiet – just clear your mind and listen. Vary hand and finger pressure, slightly, to achieve maximum contact. Have the patient breathe deeply and slowly to sense the changing pressures in the head, then stop breathing for the remaining PRM motion (ca. 10-14 cycles/minute). Don’t try to feel something. The PRM is present there and tension the physician creates by trying to feel will block the sensation. The physician should constantly monitor the tensions in their own body – fingers, wrists, elbows, shoulders, neck – and adjust for optimal comfort as tension in these areas will block the sensation. The physician should remember to stay clear and quiet in their mind – just open up and feel.
The vault hold is used to assess the PRM.
| Vault hold: | The patient is supine, about 8-10 inches from the edge. Physician contact on head is with fingers and palms of hands (no thumbs!) with the palms slightly molding to the head:
|
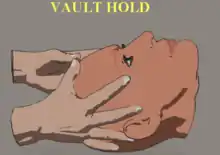 Vault Hold |
|---|
In unrestricted craniosacral motion, movement occurs around two cranial transverse axes and one sacral transverse axis at the level of S2. The sacrum has opposite motion to cranial respiration. The physiologic motions of flexion and extension were introduced in the prior section. To review, in flexion the sphenobasilar symphysis (SBS) moves upward and in extension the SBS moved downward. Cranial somatic dysfunctions are also referred to as sphenobasilar strains. These can be divided into physiologic dysfunctions – which include flexion dysfunction, extension dysfunction, left or right torsion dysfunctions, and left or right sidebending-rotation dysfunctions – or non-physiologic dysfunctions – which include left or right vertical strains, left or right lateral strains, and compression. Utilizing the vault hold, these dysfunction patterns can be identified. Physiologic dysfunctions are expected physiologic motions and can be pathological if restricted in one extreme or another.
Physiologic dysfunctions also include torsion dysfunctions, which are rotations of the SBS along an anteroposterior (AP) axis with the sphenoid and occiput rotating in opposite directions and are named for the high greater wing of the sphenoid. Sidebending-rotation dysfunctions occur around three axes: sidebending of the sphenoid and occiput occurs around two vertical axes through the body of the sphenoid at the sella turcica and the foramen magnum in opposite directions and rotation of the sphenoid and occiput around an AP axis in the same direction. This dysfunction is named for the side of convexity of the sidebending curve. Rotation occurs toward the side of convexity of sidebending.
Non-physiologic dysfunctions typically occur as a result of trauma. Vertical strains are non-physiologic shifting of the basisphenoid (base of the sphenoid) superiorly or inferiorly in relation to the basiocciput (base of the occiput). Dysfunctions are named for the base of the sphenoid in relation to the occiput. The transverse axes of rotation are through the body of the sphenoid and the occiput at the level of the jugular process. Lateral strains are non-physiologic side-to-side shearing of the SBS caused by trauma lateral to one side of the cranium, causing the sphenoid and the occiput to rotate in the same direction about vertical axes passing through the body of the sphenoid and the foramen magnum. In a compression strain, post-traumatic compression of the SBS results in restriction of all motions of the joint. Phantom hands in the vault hold will not show any appreciable motion (akin to holding a bowling ball).
Phantom hands demonstrate cranial motions.
| Cranial somatic dysfunction | Axes involved and relative motions | Schematic diagram | Phantom hands description | Phantom hands diagram |
|---|---|---|---|---|
| Flexion | Opposite rotation of the sphenoid and occiput about two transverse axes passing through sphenoid and occiput | 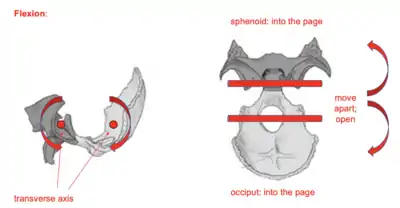 Flexion Cranial Somatic Dysfunction Bone Motion |
Fingers move away from physician and spread apart | 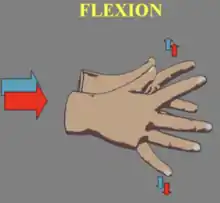 Flexion Phantom Hands Movement |
| Extension | Opposite rotation of the sphenoid and occiput about two transverse axes passing through sphenoid and occiput | 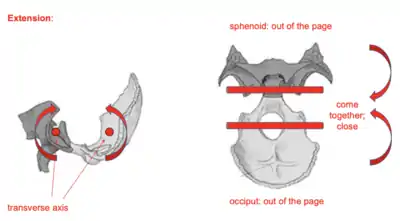 Extension Cranial Somatic Dysfunction Bone Motion |
Fingers move toward physician and come together | 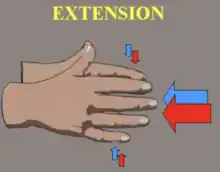 Extension Phantom Hands Movement |
| Torsion | The sphenoid and occiput rotate in opposite directions around an anteroposterior (AP) axis | 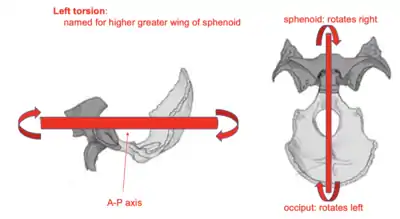 Left Torsion Cranial Somatic Dysfunction Bone Motion |
Relative to the dysfunctional side:
|
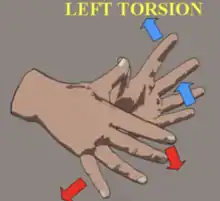 Left Torsion Phantom Hands Movement |
| Sidebending-Rotation | The sphenoid and occiput rotate about two vertical axes in opposite directions and in the same direction about an anteroposterior (AP) axis | 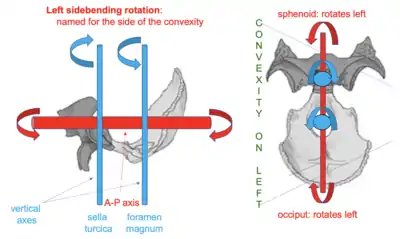 Left Sidebending-Rotation Cranial Somatic Dysfunction Bone Motion |
Relative to the dysfunctional side:
|
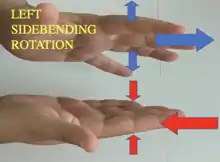 Left Sidebending-Rotation Phantom Hands Movement |
| Vertical Strain |
|
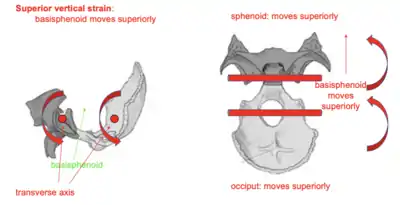 Superior Vertical Strain Bone Motion 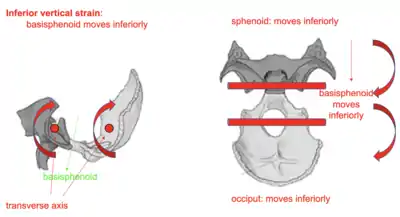 Inferior Vertical Strain Bone Motion |
|
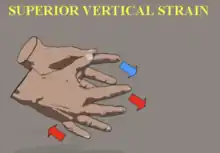 Superior Vertical Strain Phantom Hands Movement  Inferior Vertical Strain Phantom Hands Movement |
| Lateral Strain | The sphenoid and occiput rotate about two vertical axes through the sella turcica and foramen magnum leading to SBS translation | 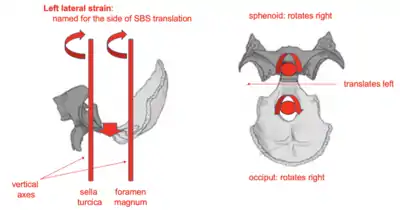 Left Lateral Strain Bone Motion |
the index fingers of both hands move to the right and the fifth digits move to the side of SBS translation | 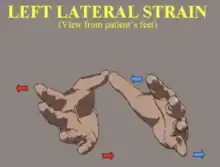 Left Lateral Strain Phantom Hands Movement |
| Compression | No motion | 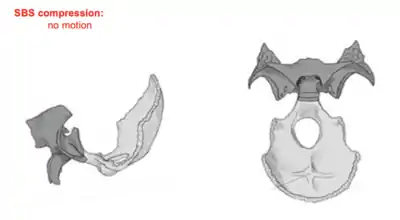 SBS Compression |
No motion | No motion |
Treatment of Cranial Somatic Dysfunctions
| Occipital condylar decompression | The patient is supine. The physician's index and middle fingers approsimate the condylar processes and initiate a gentle cephalad and lateral force. |  Occipital Condylar Decompression |
|---|---|---|
| Compression of the fourth ventricle | The patient is supine. The physician interlaces the fingers of both hands and cradles the occiput. The thenar eminences are placed posteromedially to the occipitomastoid sutures and encourages extension of the occiput while resisting flexion. The force is held until a sense of softening is felt. | .png.webp) Compression of the Fourth Ventricle (CV4) |
| Interparietal suture opening | The patient is supine. The physician's thumbs are crossed over the sagittal suture anterior and superior to lambda. The remainder of the fingers are on the lateral surfaces of the parietal bones. The crossed thumbs exert a force separating the parietal bones at the sagittal suture. This is repeated along the length of the sagittal suture to bregma. |  Interparietal Suture Opening |
| Occipitomastoid suture spread (direction of fluid) | The patient lies supine. The physician places the index and middle finvers on the two sides of the restricted suutre. As lightly as possible, the physician directs an impulse toward the restricted suture with the opposite hand cradling the suture. A "fluid wave" is perceived to be travelling the hands. |  Direction of Flow |
| Unilateral temporal rocking | The patient lies supine. The physician cradles the occiput with one hand and, with the other hand, places the third finger in the external auditory meatus. The index and thumb fingers grasp the superior aspect of the zygomatic arch and lifts cephalad. The fourth and fifth fingers exerts medial pressure to encourage external rotation of the temporal bone while the physician resists internal rotation. |  Temporal Rocking |
| Frontal lift | The patient is supine. The physician places both hypothenar eminences on the lateral angles of the front bones and the thenar eminences on the lateral aspects of the coronal suture. The fingers are interlaced above the metopic suture. The thenar and hypothenar eminences provide a gentle compressive force medially to internally rotate the frontal bones, disengaging them from the parietal bones. |  Frontal Release |
| Pareital lift | The patient is supine. The physician places the fingertips on both pareital bones and crosses the thumbs just above the sagittal suture, pressing one thumb against the other to provoke internal rotation of the parietal bones. The phsyician then lifts both hands cephalad until fullness is felt over the fingertips, thus inducing external rotation of the parietal bones. |  Parietal Lift |
Review Questions
Questions 1-5: Match the following cranial somatic dysfunction to the corresponding axes of rotation.
1. Vertical strain
2. Torsion
3. Sidebending rotation
4. Compression
5. Lateral strain
A. Rotation in the same direction around an anterior-posterior axis paired with rotation in opposite directions around two vertical axes through the foramen magnum and the body of the sphenoid.
B. The sphenoid and the occiput rotate in opposite directions around an anterior-posterior axis.
C. The sphenoid and occiput rotate in the same direction around two vertical axes through the foramen magnum and the body of the sphenoid.
D. The sphenoid and occiput rotate in the same direction around two transverse axes through the body of the sphenoid and the occiput at the level of the jugular process.
E. No apparent motion.
Questions 6-10: Match the following cranial somatic dysfunction to the corresponding phantom hand descriptions.
6. The right hand moves forward, and the fingers separate while the left hand moves backward and the fingers close.
7. The left hand rotates forward, and the fingers point down while the right hand rotates backward, and the fingers point up.
8. Both hands move backward while fingers close.
9. Both index fingers move to the right and both pinky fingers point to the left.
10. Both hands rotate forward, and the fingers point down to the floor.
11. While performing a vault hold on a patient, it is observed during cranial flexion that the left temporal bone does not move as well during extension as it does during flexion. Which of the following best describes the setup for this treatment technique?
A. The physician cradles the occiput with one hand and, with the other hand, places the third finger in the external auditory meatus. The index and thumb fingers grasp the superior aspect of the zygomatic arch and lifts cephalad. The fourth and fifth fingers exerts medial pressure to encourage external rotation of the temporal bone while the physician resists internal rotation
B. The physician resists flexion by holding occiput in extension with bilateral medial forces but not forcing into extension; the thenar eminences are placed at the squama of the occiput below the superior nuchal line leading to compression of the fourth ventricle
C. The index fingers of the hands contact the greater wings of the sphenoid bone bilaterally, the middle two fingers contact the temporal bones, and the pinky fingers contact the occiput
D. The hands are applied to the head by placing slight pressure medial and anterior to lift frontal bones and held until lateral angles of frontal bones move into external rotation
E. The physician places their index and middle fingers as a V separating the occipitomastoid suture; other hand is on opposite pole of cranium. Two fingers on one hand are placed on either side of a suture and two fingers are placed on the point that is the greatest distance away from the suture on the contralateral side
Answers to Review Questions
- D
- B
- A
- E
- C
- D
- E
- B
- H
- I
- A