Superior gluteal nerve
The superior gluteal nerve is a mixed (motor and sensory) nerve of the sacral plexus that originates in the pelvis. It provides motor innervation to the gluteus medius, gluteus minimus, tensor fasciae latae, and piriformis muscles; it also has a cutaneous branch.
| Superior gluteal nerve | |
|---|---|
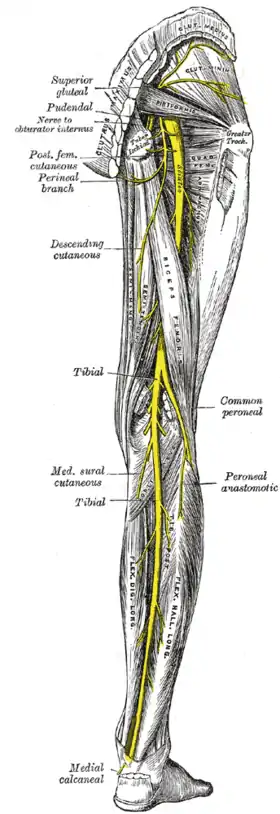 Nerves of the right lower extremity. Posterior view. | |
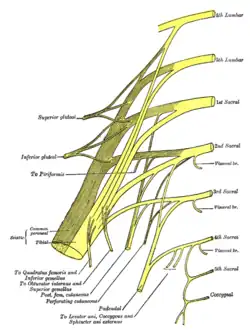 Plan of sacral and pudendal plexuses. (Superior gluteal labeled at upper left.) | |
| Details | |
| From | Sacral plexus (L4-S1) |
| Innervates | Gluteus medius, gluteus minimus, tensor fasciæ latæ |
| Identifiers | |
| Latin | Nervus gluteus superior |
| TA98 | A14.2.07.031 |
| TA2 | 6543 |
| FMA | 16510 |
| Anatomical terms of neuroanatomy | |
Structure
Origin
The superior gluteal nerve originates in the sacral plexus. It arises from the posterior divisions of L4, L5 and S1.[1]
Course
It exits the pelvis through the greater sciatic foramen superior to the piriformis muscle.[2][3][4] It is accompanied by the superior gluteal artery and the superior gluteal vein.[2]
It passes lateral-ward in between the gluteus medius muscle and the gluteus minimus muscle,[1][5] accompanied by the deep branch of the superior gluteal artery. It divides into a superior branch and an inferior branch.[5][1]
The inferior branch continues to pass between the two muscles[5] to end in the tensor fasciae latae muscle.[1]
Motor
- tensor fasciae latae muscle[6][5]
- gluteus medius muscle (superior branch and inferior branch)[1][5]
- gluteus minimus muscle (inferior branch,[1][5] sometimes superior branch as well[1])[1][5]
- piriformis muscle[7]
Sensory
The superior gluteal nerve also has a cutaneous branch.[1]
Clinical significance
Gait
In normal gait, the small gluteal muscles on the stance side can stabilize the pelvis in the coronal plane. Weakness or paralysis of these muscles caused by a damaged superior gluteal nerve can result in a weak abduction in the affected hip joint. This gait disturbance is known as Trendelenburg gait. In a positive Trendelenburg's sign the pelvis sags toward the normal unsupported side (the swing leg). The opposite, when the pelvis is elevated on the swing side, is known as Duchenne limp. Bilateral loss of the small gluteal muscles results in a waddling gait.[2]
Iatrogenic damage
The superior gluteal nerve may be damaged by intramuscular injections and nephrectomy.[3]
References
![]() This article incorporates text in the public domain from page 959 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 959 of the 20th edition of Gray's Anatomy (1918)
- Mirjalili, S. Ali (2015-01-01), Tubbs, R. Shane; Rizk, Elias; Shoja, Mohammadali M.; Loukas, Marios (eds.), "Chapter 46 - Anatomy of the Sacral Plexus L4-S4", Nerves and Nerve Injuries, San Diego: Academic Press, pp. 619–626, doi:10.1016/b978-0-12-410390-0.00048-2, ISBN 978-0-12-410390-0, retrieved 2021-02-28
- Thieme Atlas of Anatomy (2006), p 476
- David, William S.; Sadjadi, Reza (2019-01-01), Levin, Kerry H.; Chauvel, Patrick (eds.), "Chapter 13 - Clinical neurophysiology of lower extremity focal neuropathies", Handbook of Clinical Neurology, Clinical Neurophysiology: Diseases and Disorders, Elsevier, 161: 207–216, doi:10.1016/b978-0-444-64142-7.00050-3, ISBN 9780444641427, PMID 31307602, S2CID 196812589, retrieved 2021-02-28
- Moore, Keith L.; Dalley, Arthur F.; Agur, Anne M. R. (2017). Essential Clinical Anatomy. Lippincott Williams & Wilkins. p. 586. ISBN 978-1496347213.
- Moore, Keith L.; Dalley, Arthur F.; Agur, Anne M. R. (2018). Clinically Oriented Anatomy (8th ed.). Wolters Kluwer. p. 733. ISBN 978-1-4963-4721-3.
- Platzer (2004), p 420
- Iwanaga J; Eid S; Simonds E; Schumacher M; Loukas M; Tubbs RS (2019). "The Majority of Piriformis Muscles are Innervated by the Superior Gluteal Nerve". Clinical Anatomy. 32 (2): 282–286. doi:10.1002/ca.23311. PMID 30408241. S2CID 53238082.
Bibliography
- Platzer, Werner (2004). Color Atlas of Human Anatomy, Vol. 1: Locomotor System (5th ed.). Thieme. ISBN 3-13-533305-1.
- Thieme Atlas of Anatomy: General Anatomy and Musculoskeletal System. Thieme. 2006. ISBN 1-58890-419-9.
External links
- Superior gluteal nerve at the Duke University Health System's Orthopedics program