Neurocardiology
Neurocardiology is the study of the neurophysiological, neurological and neuroanatomical aspects of cardiology, including especially the neurological origins of cardiac disorders.[1] The effects of stress on the heart are studied in terms of the heart's interactions with both the peripheral nervous system and the central nervous system.
Clinical issues in neurocardiology include hypoxic-ischemic brain injury, neurogenic stress cardiomyopathy, cerebral embolism, encephalopathy, neurologic sequelae of cardiac and thoracic surgery and cardiac interventions, and cardiovascular findings in patients with primary neurological disease.[2]
Overview
Neurocardiology refers to the pathophysiological interplays of the nervous and cardiovascular systems.[3] The constant communication between the heart and the brain have proved invaluable to interdisciplinary fields of neurological and cardiac diseases.[4]
The fundamental understanding of the communication between the heart and the brain via the nervous system has led scientists into understanding its elaborate circuitry. The brain emits neurological signals of oscillating frequencies. The neural rhythms provide information on steady state conditions of healthy individuals. Variations in the neural rhythms provide evidence that a problem is present regarding physiologic regulation and help physicians determine the underlying condition quicker based on the given symptoms.[5]
The neurocardiac axis links the cardiovascular and nervous systems to physiological problems such as: arrhythmias, epilepsy, and stroke. These problems are related to the fundamental factor of stress on the body. As stated previously, the changes in neural oscillations can contribute to the knowledge of what a steady state in an individual looks like, especially because it changes based on the person, as well as contributing to the imbalance of the nervous system and physiological function. Moreover, the brain can control the heart rate through the sympathetic nervous system.[5]
Map between cardiovascular system to nervous system
The cardiovascular system is regulated by the autonomic nervous system, which includes the sympathetic and parasympathetic nervous systems. A distinct balance between these systems is crucial for the pathophysiology of cardiovascular disease. An imbalance can be caused by hormone levels, lifestyle, environmental stressors, and injuries.[6]
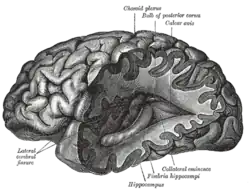
The complicated link between the brain and the heart can be mapped out from the complex of higher nervous system influences descending down to the heart. This complex innervates key autonomic structures from the brain's cortex to the heart along the neurocardiac axis. The heart is both the source of life and a source of cardiac arrhythmias and complications. The information originates in the brain's cortex and descends down to the hypothalamus. The neural signals are then transferred to the brainstem, followed by the spinal cord, which is the location where the heart receives all its signals from. In further detail, the heart receives its neural input through parasympathetic and sympathetic ganglia and lateral grey column of the spinal cord.[7]
Problems
The neurocardiac axis is the link to many problems regarding the physiological functions of the body. This includes cardiac ischemia, stroke, epilepsy, and most importantly, heart arrhythmias and cardiac myopathies. Many of these problems are due to the imbalance of the nervous system, resulting in symptoms that affect both the heart and the brain.[6]
The connection between the cardiovascular and nervous system has brought up a concern in the training processes for medical students. Neurocardiology is the understanding that the body is interconnected and weave in and out of other systems. When training within one specialty, the doctors are more likely to associate patients' symptoms to their field. Without taking the integration into account, the doctor can consequently delay a correct diagnosis and treatment for the patient.[7] However, by specializing in a field, advancement in medicine continues as new findings come into perspective.
Stress

Cardiovascular systems are regulated by the autonomic nervous systems, which includes the sympathetic and parasympathetic nervous systems. A distinct balance between these two systems is crucial for the pathophysiology of cardiovascular disease. Chronic stress has been widely studied on its effects of the body resulting in an elevated heart rate (HR), reduced HR variability, elevated sympathetic tone, and intensified cardiovascular activity. Consequently, stress promotes an autonomic imbalance in favor of the sympathetic nervous system. The activation of the sympathetic nervous system contributes to endothelial dysfunction, hypertension, atherosclerosis, insulin resistance, and increased incidence of arrhythmias.[6] An imbalance in the autonomic nervous system has been documented in mood disorders; It is commonly regarded as a mediator between mood disorders and cardiovascular disorders.
The hypothalamus is the part of the brain that regulates function and responds to stress. When the brain perceives environmental danger, the amygdala fires a nerve impulse to the hypothalamus to initiate the body's fight-or-flight mode through the sympathetic nervous system. The stress response starts with the hypothalamus stimulating the pituitary gland, which releases the adrenocorticotropic hormone. This signals the release of cortisol, the stress hormone, initiating a multitude of physical effects on the body to aid in survival. The negative feedback loop is then needed to return the body to its resting state by signaling the parasympathetic nervous system.[8]
Prolonged stress leads to many hazards within the nervous system. Various hormones and glands become overworked, chemical waste is produced resulting in degeneration of nerve cells. The result of prolonged stress is the breakdown of the body and the nervous system. Stress alone does not produce potentially deadly arrhythmias in normal healthy hearts, however studies do appear to show that stress causes cardiac damage that may lead to arrhythmias.
Arrhythmias
In a study relating to relationship of neurocardiology of arrhythmias and sudden cardiac death, they hypothesized that the individual with a diseased heart has a greater likelihood of experiencing cardiac arrhythmias and sudden cardiac death when the neurocardiac axis is activated.[7] An arrhythmia is defined as any disturbance in the cardiac activation sequence or any deviation from accepted limits of rate or regularity of the normal impulse. The main types of arrhythmia leading to sudden cardiac death are tachyarrhythmias and bradyarrhythmias. Tachyarrhythmias are associated with ventricular fibrillation and ventricular tachycardia. Bradyarrhythmias are associated with complete atrioventricular blockage and sudden asystole. The underlying cause of sudden cardiac death is unclear, despite the understanding that heart disease causes arrhythmias, which in turn produce sudden cardiac death.[7] Lown describes the heart as the target, and the brain is called the trigger. Sudden cardiac death is triggered by an electrical accident, which can be treated with ventricular defibrillation.[9]
Stroke
Stroke activates the neurocardiac axis, producing arrhythmias, cardiac damage, and sudden death. In a recent study on patients with already diseased hearts and electrocardiographic abnormalities, there was evidence of lost hypothalamic-medullary integration at the midbrain. This resulted in the fact that overactivity in the parasympathetic nervous system may also cause sudden death with asystole after stroke. Catecholamine medications have been studied to mediate the effects of electrocardiographic changes and heart damage.[7]
Epilepsy
Sudden death from epilepsy is not very common, with a rate of approximately 2 in a thousand. The present understanding about how sudden cardiac death can result from epilepsy is that the brain is stimulating an arrhythmia. Recordings during seizures report that the onset of tachycardia just prior to the seizure is common, with both atrial and ventricular ectopy.[7] The sudden epileptic death may be a result of the sympathetic activation or autonomic imbalance of the nervous system as described earlier.
Emotions
The relationship between emotions and their effect on the destabilization of the heart continues to be a mystery. It is considered that both the spatial and temporal patterns of autonomic input to the heart play a key role in altered electrophysiological parameters. The body continually attempts to maintain homeostasis through the baroreflex. This balance in the autonomic neural input to the heart in response to the pressure and volume changes leads to alterations in the baroreceptors.[10]
Treatments
Medications
Drugs with both antidepressant and cardiometabolic actions are in the process of being studied. Most of the medications work on stressors of the heart and some also work to treat the neuropsychiatric diseases. Antidepressant medications have shown to be insufficient to induce normalization of the cardiovascular dysfunctions, which are associated with the psychiatric conditions.[11]
- Hypercatecholaminergic medications[11]
- Adrenoreceptor blockers (alpha and beta)
They are most commonly used to treat hypercatecholaminergic states. Overall the blockers reduce incidences of long-term disease. The blockade not only affects cardiomyocytes directly but also works to reduce the risks of heart failure and hypertension. One side effect is that it can activate pulmonary edema with patients who unstable hearts. In particular, beta-blockers are used for the management of cardiac arrhythmias. They link the brain and the cardiovascular system in cardiovascular diseases.[6] Beta-blockers have also been studied in depressed patients. A meta-analysis concluded that with anti-depressant medication, the percentage of patients in remission from depressed symptoms significantly increased from just anti-depressants alone.[6] This suggests that this type of medication might be beneficial for both behavioral and cardiovascular symptoms of depression. - Aldosterone antagonist
- Spironolactone
This medication acts by inhibiting binding to mineralocorticoid receptors. This has shown positive feedback in tackling both cardiovascular and activation of the main feature of stress-related disorders.[6] Aldosterone antagonists are usually a form of combined treatment with other cardiac medications, but it appears to induce favorable sympathovagal balance. Some side effects of Spironolactone are hyperkalemia, erectile dysfunction, lower testosterone levels, and menstrual irregularities, all of which lead to an increase in noncompliance with the medication.[12]
- Spironolactone
- Adrenoreceptor agonist
- Clonidine
Acts on the central nervous system to inhibit the sympathetic nervous system, leading to a decrease in blood pressure. It is commonly used to reduce the risk of stroke and heart attacks by treating high blood pressure, anxiety, and panic disorders. It also leads to the decreased activity of norepinephrine release from the sympathetic nerve terminals.[11]
- Clonidine
- Adrenoreceptor blockers (alpha and beta)
Physical activity and diet
Lifestyle modifications play a crucial role in management of cardiovascular and neurological diseases. Physical activity and a well-balanced diet favor cardiovascular conditioning and improves performance and capacity. Exercise has a positive effect on the metabolism, which controls glucose levels, especially for stress-related pathology and brain disorders such as depression, which impose a heavy burden on the cardiovascular system. Many studies are currently being done for more information and knowledge regarding the common mediators for cardiovascular disease and the central nervous system. The brain-heart interaction is considered bidirectional, however the majority of times the central nervous system is regulated more over the heart and blood vessels.[6]
See also
References
- Natelson BH (Feb 1985). "Neurocardiology. An interdisciplinary area for the 80s". Arch. Neurol. 42 (2): 178–84. doi:10.1001/archneur.1985.04060020096022. PMID 3883960.
- Louis R Caplan; J Willis Hurst; Marc I Chimowitz (1999). Clinical neurocardiology. p. 324. doi:10.1201/b14098. ISBN 9780429074516. PMC 325678.
{{cite book}}:|journal=ignored (help) - van der Wall, E; W.H. van Gilst (December 2012). "Neurocardiology: close interaction between heart and brain". Netherlands Heart Journal. 21 (2): 51–52. doi:10.1007/s12471-012-0369-4. PMC 3547430. PMID 23239452.
- Carrero, Milton (12 February 2011). "One Vital Organ: Heart is More than a Pump". The Morning Call.
- Fallen, Ernest (December 2000). "Hidden rhythms in the heart record: a primer on neurocardiology". Clin Invest Med. 23 (6): 387–394. PMID 11152408.
- Pereira, VH; Cerqueira, JJ; Palha, JA; Sousa, N (5 June 2013). "Stressed brain, diseased heart: a review on the pathophysiologic mechanisms of neurocardiology". International Journal of Cardiology. 166 (1): 30–37. doi:10.1016/j.ijcard.2012.03.165. hdl:1822/24143. PMID 22521375.
- Davis, Alan (1993). "Brain-Heart Interactions: The Neurocardiology of Arrhythmia and Sudden Cardiac Death". Texas Heart Institute Journal. 20 (3): 158–169. PMC 325088. PMID 8219819.
- "How Your nervous System Gets Out of Sync" (PDF). Retrieved 28 October 2013.
- Lown, B; Verrier RL; Rabinowitz SH (May 1977). "Neural and Psychologic Mechanisms and the Problem of Sudden Cardiac Death". American Journal of Cardiology. 39 (6): 890–902. doi:10.1016/s0002-9149(77)80044-1. PMID 860697.
- Taggart, Peter; Mark Boyett; Sunil Logantha; Pier Lambiase (October 2011). "Anger, Emotion, and Arrhythmias: from Brain to Heart". Frontiers in Physiology. 2: 67. doi:10.3389/fphys.2011.00067. PMC 3196868. PMID 22022314.
- Goldstein, David S. (2012). "Neurocardiology: Therapeutic Implications for Cardiovascular Disease". Cardiovascular Therapeutics. 30 (2): 89–106. doi:10.1111/j.1755-5922.2010.00244.x. PMC 4893308. PMID 21108771.
- Maron, Bradley (2010). "Aldosterone Receptor Antagonists: Effective but Often Forgotten". Circulation. 121 (7): 934–939. doi:10.1161/CIRCULATIONAHA.109.895235. PMC 2828634. PMID 20177008.
Further reading
- Aulbert, E. A., et al.: Neurocardiology: the benefits of irregularity. The basics of methodology, physiology and current clinical applications. Acta Cardiol. 1999 (54) 107–120
- Levine RL (May 2007). "Neurocardiology". Resuscitation. 73 (2): 186–8. doi:10.1016/j.resuscitation.2007.01.012. PMID 17346869.
- Gielerak G (Jun 2007). "[Neurocardiology--contemporary advanced research concerning arrhythmia mechanisms and sudden cardiac death]". Kardiol Pol (in Polish). 65 (6): 709–14. PMID 17629835.