Chapter 10: Ambulatory Dysfunction and Falls
Objectives:
- Define basic gait terminology used for measurement and
- Define the phases of
- Discuss the impact of ambulatory dysfunction and falls on functional status
- Describe pathologic gait patterns
- Describe causes and mechanisms of syncope and hypotension
- Describe the disease process, diagnosis, and treatment of osteoporosis and preventive screening recommendations
- Describe alcohol drink equivalents
- Be able to utilize the CAGE questionnaire to screen for alcohol abuse
- Describe symptoms and treatment for Parkinson’s disease
- Describe how to perform simple gait and balance assessments
- Identify intrinsic and extrinsic causes of falling and how they affect future risks of falling
- Discuss age-related changes which can contribute to falls
- Identify factors which place a patient at risk for falls
- Describe medications which contribute to fall risk
- Describe non-pharmacologic interventions effective in decreasing falls
Gait
The bones of the spine and pelvis move in specific directions during the normal walking cycle, depending on which leg is moving forward. Dynamic motion of the sacrum and innominates occurs during walking. As weight bearing shifts to one leg, unilateral lumbar sidebending engages the ipsilateral oblique sacral axis by shifting weight to that sacroiliac joint. The sacrum now rotates forward on the opposite side, creating a deep sacral sulcus. With the next step, this process reverses as weight bearing changes to the other leg. The sacral base is constantly moving forward on one side, then the other, about the oblique axes. (Thus, physiologic somatic dysfunctions of the sacrum are named as such because these motions occur during the normal walking cycle.) As this occurs, the innominates are rotating in opposite directions to each other about the inferior transverse sacral axis (S4). One side rotates anteriorly as the other side rotates posteriorly. Summarizing: the anterior leg has a posterior innominate and an anterior sacral base with a deep sacral sulcus; the posterior leg has an anterior innominate and posterior inferior lateral angle. Figure 10.1 illustrates the gait cycle and reflects both new and classic terminology.
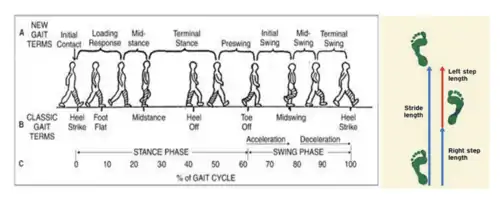
Figure 10.1 – Gait Cycle Terminology; graphical representation of stride and step lengths (source unknown)
The gait cycle is the sequence of functions of one limb. One gait cycle is equal to one stride, and one stride length is equal to two steps. The stance phase occurs when the limb is in contact with the ground. The swing phase occurs during limb advancement and limb clearance. The stance phase involves initial contact, loading response, mid-stance, terminal stance, and preswing. As walking speed increases, the stance phase decreases and the swing phase increases. Cadence describes the number of steps per unit time or distance.
During the loading response, weight shifts to the stance leg when the contralateral limb is lifting off the ground; this is where the lowest center of gravity is present. During the midstance phase, the ankles are aligned in the coronal plane; this is where the highest center of gravity is present. (The center of gravity is located 5 cm anteriorly to S2.) The terminal stance occurs after the midstance and just prior to the initial contact of the contralateral limb. During preswing, unloading of the ipsilateral limb occurs just prior to lift off. To permit the body to move forward on the right, trunk rotation in the thoracic area occurs to the left accompanied by lateral flexion to the left in the lumbar with movement of the lumbar vertebrae into the forming convexity to the right (the thoracic spine rotates left and the lumbar spine sidebends left and rotates right). There is a torsional locking at the lumbosacral junction on the left as the body of the sacrum is moving to the left, about a left oblique axis (L on L), thus shifting the weight of the body to the left foot to allow lifting of the right foot. The shifting vertical center of gravity moves to the superior pole of the left sacroiliac, locking the mechanism into mechanical position to establish movement of the sacrum on the left oblique axis which sets the pattern so the sacrum can torsionally turn to the left. The sacral base moves down (deep) on the right to conform to the lumbar C curve that is now formed to the right (lumbar spine is rotated right, convex right or sidebent left). The sacrum rotates in the opposite direction (to the left) of the lumbar spine (to the right). When the right foot moves forward, there is tensing of the right quadriceps and accumulating tension at the inferior pole of the right sacroiliac at the junction of the left oblique axis and the inferior transverse axis, which eventually locks as the weight swings forward allowing slight anterior movement of the right innominate on the inferior transverse axis. The movement is increased by the backward thrust of the restraining ground on the right leg.
The swing phase involves the initial swing, mid-swing, and the terminal swing phases. The initial swing involves lifting the limb off ground to maximum knee flexion. Tension on the hamstrings begins as the weight swings upward to the crest of the femoral support and there is a slight posterior movement of the right innominate on the inferior transverse axis. The movement is further increased by the weight of forward thrust of the propelling leg action. As the right heel strikes the ground, trunk torsion and accommodation begin to reverse themselves. As the left foot passes the right and weight passes over the crest of the femoral support, and accumulating force from above moves to the right, the sacrum changes its axis to the right oblique axis and the left sacral base moves forward towards the right around the right oblique axis. (R on R)
The mid-swing phase involves maximum knee flexion vertically to the tibia. During this phase, the left innominate moves from anterior rotation to posterior. The sacrum rotates rightward on a right oblique axis. The right anterior rotates anteriorly. (Summarizing, when the left leg is coming forward, the right innominate is anterior, the left innominate is posterior, and the sacrum is rotated right on a right oblique axis.) The terminal swing describes the vertical tibia position to just prior to initial contact. Double-limb support is present at the beginning and end of stance phase (20% of the gait cycle); single-limb support during swing phase (80% of the gait cycle). Running offers no double-limb support.
The six determinants of gait include:
- Pelvic rotation
- Pelvic tilt
- Lateral displacement of the pelvis
- Knee flexion in the stance phase
- Knee mechanisms
- Foot mechanisms
These determinants and any aberrations of them contribute to gait pathology.
- Gluteus medius gait (Trendelenburg gait) involves a shift of the body toward the deficient side, indicating a weakness of the gluteus medius muscle and can be identified by a positive Trendelenburg sign in the upright position.
- Gluteus maximus gait involves the trunk and pelvis being hyperextended backward over both hips to maintain the center of gravity behind the involved hip joint. A short lower extremity results in the pelvis and trunk being depressed in the stance phase.
- Waddling gait occurs due to an elevated pelvis gait occurs from a hiking or if elevation of the pelvis on the swing side if the hip or knee motion is limited. Congenital hip dislocation will manifest as a waddling gait.
- Osteoarthrosis gait occurs secondary to severe osteoarthrosis of the hip or knee joints and results in a “scissoring” gait. Any foot dysfunction may alter normal mechanics. These could include Morton's neuroma, corns, calluses, bunions, hallux rigidus, plantar warts, or poorly fitting shoes. If plantar flexion is absent, there is no push-off and the heel and forefoot come off the floor together.
- Hemiplegic gait: The affected leg is usually stiff, with loss of flexion at the hip and knee joints. The patient leans to the affected side and throws the whole leg outward from the body before bringing it back toward the trunk, producing a circumduction movement. The shoe is dragged against the floor, and there is usually an accompanying affected arm that does not swing but is held in fixed position against the abdomen with the elbow flexed.
- High-steppage gait: There are two patterns – the first pattern and the second pattern. In the first pattern, the toe touches the floor first, with a foot drop caused by paralysis of pretibial or peroneal muscles. The leg is raised high by abnormal knee and hip flexion. The toe touches the ground first, followed by a slapping noise as the foot strikes the floor. In the second pattern, the heel touches the floor first because of loss of sense of position. The high-steppage gait is bilateral, with ataxia and side-to-side reeling. The heel touches the floor first and a stomp of the foot is heard. Romberg sign is present, caused by a dysfunction of the afferent portion of peripheral nerves or posterior roots. Carcinoma, diabetic neuropathy, tabes dorsalis, Friedreich's ataxia, subacute combined degeneration of the cord, compression lesions of the posterior columns, and multiple sclerosis that affects the posterior columns may all produce a high-steppage gait.
- Shuffling gait: Shuffling gait is identified by small, flat-footed shuffling steps; the foot does not clear the ground. In Parkinsonism, rigidity, tremor, paucity of movement, shuffling with haste, and difficulty in starting, stopping, or turning are noted. The patient is in truncal flexion, with lack of extension movements at the hips, knees, and elbows. The thorax and pelvis rotate in the same direction in swing phase. The amplitude of vertical excursions of the head is lessened in forward motion. The first noticeable motor signs in Parkinsonism may be a non-rhythmic pattern with random or poorly timed activity of the arms in gait. Due to loss of confidence and equilibrium, the patient stands erect, takes small shuffling steps with a wide base, and seems to stare at a distant point. Turning is achieved through a series of small steps made by one foot, the other foot acting as a pivot.
- Ataxic gait: A reeling, unsteady gait with a wide base and a tendency to fall toward the side of the lesion. Vertigo may accompany ataxia. It may be found in cerebellar disease, multiple sclerosis, and sometimes myxedema. Ataxic gait must be differentiated from drunken and staggering gait, in which the subject reels, totters, tips forward and backward, and may lose balance and fall. This gait is seen in alcohol or barbiturate poisoning, drug reaction, polyneuritis, or general paresis.
- Scissors gait: The legs are adducted, crossing alternately in front of one another. Both lower limbs are spastic, and there is spasm of the adductor muscles at the hip joints, often accompanied by pronounced compensatory motions of the trunk and upper extremities. Bilateral upper motor neuron lesions, advanced cervical spondylosis, or multiple sclerosis may produce this gait pattern.
- Waddling gait: Rolling from side to side, the pelvic rotation and tilt on the swing side are increased (“penguin walk”). Muscular dystrophy with weakness of hips, exaggerated lordosis, and pot-bellied posture can produce this gait.
Ambulatory Dysfunction and Falls
Ambulatory dysfunction is characterized by a physical and permanent disability to such a degree that the person is unable to move from place to place without the aid of an assistive device. Causes of ambulatory dysfunction are multifactorial and can be caused by the pathologic gait functions as described above or by physical deconditioning and debility. Statistically, persons age 65 or older have a 30% incidence of falls each year, and persons age 80 or older have a 50% incidence. Half of those who fall have fallen multiple times. The most common consequence of ambulatory dysfunction is a fall. The best predictor of a fall is a history of previous falls. Most falls do not result in injury, but consequences of falls include physical injury and bruising, loss of consciousness, and rhabdomyolysis if the patient is on the ground or stuck in one position for a long period of time due to constant muscle contraction leading to breakdown.
As discussed in Chapter 3, inquiring about falls and fall risk reduction is essential and necessary. Fall risk/reduction: How many falls has the patient had? Does the patient utilize an ambulatory device? Is the patient receiving physical or occupational therapy, or involved in a restorative nursing program? Does home have grab bars in bathroom, handrails on stairs, adequate lighting, and secured rugs?
Ambulatory dysfunction is evaluated in the in-patient and also the rehabilitation setting by physical therapists. Causes of ambulatory dysfunction and falls may be due to physical deconditioning, disease processes, or secondary to medication use. Treatment of ambulatory dysfunction is paramount due to the foreshadowed impact on functional decline. Other factors considered in subsequent sections that may contribute to falls include alcohol abuse, Parkinson’s disease, syncope and hypotension, and the consequences of falls in patients with.
As part of the physical exam, in addition to heart, lungs, and abdomen assessments, one should also evaluate neurologic evaluation including muscle strength of the upper and lower extremities, deep tendon reflexes of the upper and lower extremities, coordination testing including finger-to-nose, heel-to-shin, and tandem i.e. heel-to-toe (“sobriety test”) walking, timed get-up-and-go testing, and, as appropriate, cognitive testing (MOCA, digit span, orientation, etc.). The timed get up and go test is used to assess a person's mobility and requires both static and dynamic balance. It uses the time that a person takes to rise from a chair without assistance, walk three meters, turn around, walk back to the chair, and sit down. If the total time to perform this time is less than 10 seconds, the risk of falling in this patient is considered low. If the time is between 10-20 seconds, the risk of falling is intermediate. If the time required is greater than 20 seconds, the patient is at a high risk of falling. The Tinetti Gait and Balance Assessment can also be used to assess fall risk. The instrument can be reviewed and downloaded from the provided hyperlink.
Alcohol Abuse
Alcohol abuse is associated with falls and cognitive impairment, as well as other issues such as macrocytic anemia, B12 deficiency, electrolyte derangement, and poor oral intake.
One drink is defined as:
- 12 fluid ounces of beer
- 8 fluid ounces of malt liquor
- 4 fluid ounces of wine
- 1.5 fluid ounces of 80-proof hard liquor
In patients with suspected alcohol abuse, utilizing the CAGE questionnaire is appropriate:
- Have you ever felt the need to Cut back on your drinking?
- Have people Annoyed you by criticizing your drinking?
- Have you ever felt Guilty about drinking?
- Have you ever felt the need for an Eye-opener first thing in the morning?
Each question in the CAGE questionnaire is assigned 1 point. CAGE testing is considered positive with a score of 2 or higher. Some physicians consider the “eye opener” question as highly concerning for unhealthy drinking behavior, even if all other questions are answered negatively.
Parkinson’s Disease, Syncope, and Hypotension
Parkinson's disease was initially discussed in Chapter 5. Parkinson’s disease is clinically identified by the presence of symptoms including micrographia (small handwriting), cogwheel rigidity with joint movement (most easily appreciated by assessing pronation and supination and monitoring the radial head), resting tremor, and a short-stepped shuffling gait. First line treatment should involve initiation of carbidopa/levodopa to replete central nervous system dopamine. Incidence of Parkinson’s disease is 1 million in the United States and 10 million worldwide; prevalence is 60,000 per year in the United States.
In Lewy body dementia, cognitive impairment is a presenting feature at the time of diagnosis of Parkinson’s disease. In Parkinson’s disease dementia, cognitive impairment typically occurs in the last half of the Parkinson’s disease clinical course. Hallucinations are a hallmark feature of Lewy body dementia. Rivastigmine is indicated for Parkinson’s disease-related dementias.
Syncope is defined as a transient loss of consciousness due to insufficient cerebral perfusion. It is the result of hypotension and bradycardia leading to a sudden drop in venous return to the heart, causing an “empty ventricle” to contract, stimulating mechanoreceptors and triggering vagus nerve input. Associated prodromal symptoms include fatigue, dizziness, and headache. Symptoms after the episode may include confusion, nausea, headache, and residual dizziness.
Hypotension is an abnormally low blood pressure. Causes may be multifactorial. Particularly in the geriatric population, orthostatic hypotension, or significant changes in blood pressure with postural (i.e. positional) changes is common. Orthostatic hypotension is defined as a change in systolic blood pressure of 20 mm Hg, a change in diastolic blood pressure of 10 mm Hg within three minutes of standing when comparing the blood pressure in a supine or seated position. Orthostatic hypotension may occur due to dehydration or medications, among other causes. Blunted baroreceptor reflexes due to orthostatic hypotension can leading to an increased risk of syncope and falls.
Autonomic dysregulation associated with Parkinson’s disease will manifest as labile (hypertensive and hypotensive) blood pressures and be refractory to treatment. Treatment of hypotension can be affected by fludrocortisone and midodrine.
Post-prandial hypotension is characterized by a decrease in blood pressure of 20 mm Hg within two hours of eating. The incidence is approximately 35% of all long-term care residents. It is caused by inadequate sympathetic compensation for increased splanchnic blood flow. Treatment involves small frequent meals and restricting carbohydrates. Caffeinated beverages may also be an effective intervention.
Osteoporosis
Osteoporosis is characterized by bones that become thin, brittle, and weak. These changes can increase the risk of fractures. Fractures caused by osteoporosis have been linked to an increased risk of death. Osteoporosis is often asymptomatic. On physical and structural examinations, cervical spine compression fractures will lead to an increased thoracic kyphosis. One of the most serious consequences of a fall is a hip fracture which can occur due to a mechanical fall and be precipitated by osteoporosis. About 25% of patients who sustain a hip fracture from a fall die within 6 months. Hip fractures are the leading cause of accidental death. Almost 50% of hip fracture patients will require placement in a nursing home for sub-acute rehabilitation, and of those, 50% remain in a nursing home for long-term care. Only 30% of hip fracture patients will regain their prior functional status.
Osteoporosis occurs five times more often in women than in men. Women aged 65 and older should be screened for osteoporosis. There is no frequency for screening provided by the USPSTF guidelines. A DEXA scan is used to assess bone density for osteoporosis screening. Bone densities are assigned a T score value. A T score value of more than -2.5 standard deviations below the young adult female reference mean in the presence of one or more fragility fractures is diagnostic for osteoporosis.
Estrogen protects against bone loss. After menopause, ovaries produce little estrogen and this triggers a period of rapid bone loss in women that starts 1 year before the final menstrual period and lasts for about 3 years. The natural effects of aging on bones contributes to this bone loss as well. Treatment involves bisphosphonates, which act by preventing and slowing down bone loss, as well as calcium and vitamin D supplementation.
Review Questions
Questions 1-3: An 83-year-old female presents to her primary care physician for follow up of her chronic medical conditions. She denies any new problems or complaints. She presents to the office by herself. Her medications are amlodipine and atorvastatin. Her vital signs and physical exam are unremarkable. Her osteopathic structural exam is notable for increased thoracic kyphosis. Her recent lab studies are unremarkable. She expresses concern about a “hump” on her back and feeling “more stooped forward” in recent years.
1. Which of the following is the most appropriate treatment for the management of osteoporosis?
A. Calcium/Vitamin D supplementation
B. Bisphosphonates
C. Vertebral kyphoplasty
D. Thoracic Lumbar Sacral Orthotic (TLSO) brace
E. Laminectomy
2. The patient is prescribed a dual energy X-ray absorptiometry (DEXA) scan by her physician. The results indicate a T score of -2.8 of the femoral neck. Which of the following correctly describes the interpretation of this score?
A. The patient has a normal bone density based on the results of the DEXA scan.
B. The patient has osteopenia based on the results of the DEXA scan.
C. The patient has osteoporosis based on the results of the DEXA scan.
D. The patient likely has pathologic bone fractures secondary to metastatic cancer.
E. There is insufficient evidence to establish or rule out a diagnosis for this patient.
3. What is the significance of the increased thoracic kyphosis noted on the physical exam of this patient?
A. Her physical exam shows normal age-related changes in physiology.
B. Compression fractures of the cervical spine are the cause of increased thoracic kyphosis.
C. Compression fractures of the thoracic spine are the cause of increased thoracic kyphosis.
D. Increased thoracic kyphosis occurs due to frequent falls with recurrent injury to the cervical spine.
E. Increased thoracic kyphosis occurs due to frequent falls with recurrent injury to the thoracic spine.
Questions 4-6: A 76-year-old male presents to his primary care physician at the urging of his son for evaluation of frequent falls. He notes that he has been falling frequently. The falls are occurring at all times of the day. He notes that he feels dizzy sometimes immediately upon standing up. He has not been started on any new medications recently. He denies any head injury or loss of consciousness. He states that the symptoms began approximately four months ago. Of note, his wife passed away six months ago. He does admit to having at least three to four shots of bourbon per day because his friend gave him a bottle following the death of his wife. He notes that he drinks at varying times of the day, sometimes even when he first wakes up in the morning. His medical history is notable for hypertension and diabetes mellitus type 2. He denies any surgical history. He denies any contributing family history. His medications include amlodipine 5 mg 1 tab daily, hydrochlorothiazide 12.5 mg 1 tab daily, lisinopril 2.5 mg 1 tab daily and metformin 500 mg 1 tab with breakfast and dinner. When asked if he has any history of alcohol abuse, he denies this. He also denies any tobacco abuse history or drug use. He lives alone but he does have two sons nearby who frequently check on him. His vital signs show a blood pressure of 130/80 seated, which drops to 100/68 upon standing; heart rate of 75 seated which increased to 90 standing; temperature of 98.8 F, respiratory rate of 18, and oxygen saturation of 97%. His physical exam is notable for bruises at mild stages of resolving all over his body including on his head, chest, arms, back, and legs. His neurologic exam is unremarkable. He does show +1 bilateral lower extremity edema. The remainder of the physical exam is unremarkable.
4. How is orthostatic hypotension diagnosed?
A. A change in systolic blood pressure of 20 mm Hg or a change in diastolic blood pressure of 10 mm Hg within three minutes of sitting when comparing the blood pressure from a standing position.
B. A change in systolic blood pressure of 20 mm Hg or a change in diastolic blood pressure of 10 mm Hg within three minutes of standing when comparing the blood pressure in a supine or seated position.
C. A change in systolic blood pressure of 20 mm Hg or a change in diastolic blood pressure of 10 mm Hg within three minutes of laying in the supine position when comparing the blood pressure in a standing or seated position.
D. A sensation of dizziness reported by the patient with changing positions.
5. Which of the following interdisciplinary team referrals is most appropriate for this patient?
A. Physical therapy
B. Occupational therapy
C. Speech therapy
D. Social work referral
E. Case management referral
6. Which of the following is equivalent to one drink?
A. 8 fluid ounces of beer
B. 12 fluid ounces of malt liquor
C. 10 ounces of wine
D. 1.5 fluid ounces of 80-proof hard liquor
E. 2 mixed drinks
7. How are Parkinson's disease dementia and Lewy body dementia differentiated?
A. In Parkinson's disease dementia, cognitive impairment is a presenting feature at the time of diagnosis of Parkinson's disease
B. In Lewy body dementia, cognitive impairment typically occurs in the last half of the Parkinson's disease clinical course
C. Executive dysfunction is a hallmark feature of Parkinson's disease dementia
D. Hallucinations are a hallmark feature of Parkinson's disease dementia
E. Clonazepam is indicated for the treatment of agitation in Lewy body dementia whereas no medication is indication for agitation in Parkinson’s disease dementia
Questions 8-9: A 73-year-old male presents to his primary care physician complaining of “the shakes”. He notes that he first observed a trembling of his right hand at rest approximately six months ago and attributed it to anxiety following the recent death of his wife. He now notes the trembling in both of his hands at rest, as well as feeling “stiff”. He has had two falls in the last month. He states that “I’ve had trouble starting to walk when I first stand up, and then I lose my balance and fall over. Sometimes I feel dizzy, sometimes I don’t. My handwriting has gotten very small and hard to read too.” His medical history is notable for hypertension, hyperlipidemia, diabetes mellitus type 2, and coronary artery disease for which he underwent catheterization with stent placement. His medications include glipizide, lisinopril, atorvastatin, and amlodipine. His vital signs are unremarkable. His physical exam is notable for cogwheel rigidity, a short-stepped shuffling gait. Review of his laboratory studies indicate excellent control of his diabetes mellitus with a recent hemoglobin A1c of 7.2%.
8. What is the most likely diagnosis given the clinical presentation of this patient?
A. Cerebrovascular accident in the cerebellum
B. Diabetic peripheral neuropathy
C. Parkinson’s disease
D. Orthostatic hypotension
E. Alcohol withdrawal
9. What is the most appropriate initial treatment for this patient?
A. Stop amlodipine
B. Stop lisinopril
C. Start carbidopa/levodopa
D. Start midodrine
E. Stop glipizide
Answers to Review Questions
- B
- C
- B
- B
- A
- D
- C
- C
- C