Pulse pressure
Pulse pressure is the difference between systolic and diastolic blood pressure.[1] It is measured in millimeters of mercury (mmHg). It represents the force that the heart generates each time it contracts. Healthy pulse pressure is around 40 mmHg.[1][2] A pulse pressure that is consistently 60 mmHg or greater is likely to be associated with disease, and a pulse pressure of 50 mmHg or more increases the risk of cardiovascular disease.[1][3] Pulse pressure is considered low if it is less than 25% of the systolic. (For example, if the systolic pressure is 120 mmHg, then the pulse pressure would be considered low if it is less than 30 mmHg, since 30 is 25% of 120.)[2] A very low pulse pressure can be a symptom of disorders such as congestive heart failure.[3]
| Pulse pressure | |
|---|---|
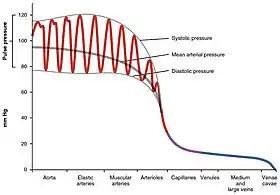 Pulse pressure variation (PPV) in different arteries and veins |
Calculation
Pulse pressure is calculated as the difference between the systolic blood pressure and the diastolic blood pressure.[3][4]
The systemic pulse pressure is approximately proportional to stroke volume, or the amount of blood ejected from the left ventricle during systole (pump action) and inversely proportional to the compliance (similar to elasticity) of the aorta.[5]
The aorta has the highest compliance in the arterial system due in part to a relatively greater proportion of elastin fibers versus smooth muscle and collagen. This serves to dampen the pulsatile (maximum pumping pressure) of the left ventricle, thereby reducing the initial systolic pulse pressure, but slightly raising the subsequent diastolic phase. If the aorta becomes rigid because of disorders, such as arteriosclerosis or atherosclerosis, the pulse pressure would be high due to less compliance of the aorta.
- Systemic pulse pressure (usually measured at upper arm artery) = Psystolic - Pdiastolic
- e.g. normal 120mmHg - 80mmHg = 40mmHg[3]
- low: 107mmHg - 80mmHg = 27mmHg
- high: 160mmHg - 80mmHg = 80mmHg
- Pulmonary pulse pressure is normally much lower than systemic blood pressure due to the higher compliance of the pulmonary system compared to the arterial circulation.[6] It is measured by right heart catheterization or may be estimated by transthoracic echocardiography Normal pulmonary artery pressure is between 8mmHg -20 mm Hg at rest.[7]
- e.g. normal: 15mmHg - 8mmHg = 7mmHg
- high: 25mmHg - 10mmHg = 15mmHg
Values and variation
Low (narrow) pulse pressure
A pulse pressure is considered abnormally low if it is less than 25% of the systolic value.[2] If the pulse pressure is extremely low, i.e. 25 mmHg or less, it may indicate low stroke volume, as in congestive heart failure.[3]
The most common cause of a low (narrow) pulse pressure is a drop in left ventricular stroke volume. In trauma, a low or narrow pulse pressure suggests significant blood loss.[8]
A narrow pulse pressure is also caused by aortic stenosis.[3]
From exercise
For most individuals, during aerobic exercise, the systolic pressure progressively increases while the diastolic pressure remains about the same, thereby widening the pulse pressure. These pressure changes facilitate an increase in stroke volume and cardiac output at a lower mean arterial pressure, enabling greater aerobic capacity and physical performance. The diastolic drop reflects a reduced systemic vascular resistance of the muscle arterioles in response to the exercise.[9]
Consistently high
A pulse pressures of 50 mmHg or more can increase the risk of heart disease, heart rhythm disorders, stroke and other cardiovascular diseases and events. Higher pulse pressures are also thought to play a role in eye and kidney damage from diseases such as diabetes.[3] If the usual resting pulse pressure is consistently greater than 100 mmHg, potential factors are stiffness of the major arteries, aortic regurgitation (a leak in the aortic valve), or arteriovenous malformation, among others.[3] While some drugs for hypertension have the side effect of increasing resting pulse pressure, other antihypertensive drugs, such as hydrochlorothiazide, have been shown to lower pulse pressure.[10] A high pulse pressure combined with bradycardia and an irregular breathing pattern is associated with increased intracranial pressure, a condition called Cushing's triad seen in people after head trauma with increased intracranial pressure.[11]
Common causes of widening pulse pressure include:[3]
Clinical significance
A vast amount of diagnostic, prognostic, and prophylactic value can be derived from the proper monitoring and interpretation of pulse pressure. Pulse pressure has implications for both cardiovascular disease as well as many non-cardiovascular diseases.
Cardiovascular disease and pulse pressure
Awareness of the effects of pulse pressure on morbidity and mortality is lacking relative to the awareness of the effects of elevated systolic and diastolic blood pressure. However, pulse pressure has usually been found to be a stronger independent predictor of cardiovascular events, especially in older populations, than has systolic, diastolic, or mean arterial pressure.[3]
A meta-analysis in 2000 showed that a 10 mmHg increase in pulse pressure was associated with a 20% increased risk of cardiovascular mortality, and a 13% increase in risk for all coronary end points. The study authors also noted that, while risks of cardiovascular end points do increase with higher systolic pressures, at any given systolic blood pressure the risk of major cardiovascular end points increases, rather than decreases, with lower diastolic levels.[13] This suggests that interventions that lower diastolic pressure without also lowering systolic pressure (and thus lowering pulse pressure) could actually be counterproductive. Increased pulse pressure is also a risk factor for the development of atrial fibrillation.[14]
Effects of medications on pulse pressure
A 2001 randomized, placebo-controlled trial of 1,292 male veterans, compared the effects of hydrochlorothiazide (a thiazide diuretic), atenolol (a beta-blocker), captopril (an ACE inhibitor), clonidine (a central α2-agonist), diltiazem (a calcium channel blocker), and prazosin (an α1-blocker) on pulse pressure and found that, after one year of treatment, hydrochlorothiazide was the most effective at lowering pulse pressure, with an average decrease of 8.6 mm Hg. Captopril and atenolol were equal as least effective, with an average decrease of 4.1 mm Hg. Clonidine (decrease of 6.3 mm Hg), diltiazem (decrease of 5.5 mm Hg), and prazosin (decrease of 5.0 mm Hg) were intermediate.[10]
Pulse pressure and sepsis
Diastolic blood pressure falls during the early stages of sepsis, causing a widening of pulse pressure. If sepsis becomes severe and hemodynamic compromise advances, the systolic pressure also decreases, causing a narrowing of pulse pressure.[15] A pulse pressure of over 70 mmHg in patients with sepsis is correlated with an increased chance of survival. A widened pulse pressure is also correlated with an increased chance that someone with sepsis will benefit from and respond to IV fluids.[16]
See also
References
- Homan TD, Bordes SJ, Cichowski E (12 July 2022). "Physiology, Pulse Pressure". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 29494015. Retrieved 2019-07-21 – via NCBI Bookshelf.
- Liaw SY, Scherpbier A, Klainin-Yobas P, Rethans JJ (September 2011). "A review of educational strategies to improve nurses' roles in recognizing and responding to deteriorating patients". International Nursing Review. 58 (3): 296–303. doi:10.1111/j.1466-7657.2011.00915.x. PMID 21848774.
- "Pulse pressure". Cleveland Clinic. 28 July 2021. Retrieved 10 February 2023.
If you check your blood pressure regularly and notice you have an unusually wide (60 mmHg or more) or narrow pulse pressure (where your pulse pressure is less than one-quarter of the top blood pressure number), you should schedule an appointment with your healthcare provider to talk about it. [...] Pulse pressures of 50 mmHg or more can increase your risk of heart disease, heart rhythm disorders, stroke and more. Higher pulse pressures are also thought to play a role in eye and kidney damage from diseases like diabetes.
- Weber CO (24 February 2022). Shah A (ed.). "Pulse Pressure". about.com. Archived from the original on 17 February 2009.
- Klabunde RE (29 March 2007). "Arterial pulse pressure". Cardiovascular Physiology Concepts. Archived from the original on 16 May 2008.
- Blacher J, Evans A, Arveiler D, et al. (January 2010). "Residual cardiovascular risk in treated hypertension and hyperlipidaemia: the PRIME Study" (PDF). Journal of Human Hypertension. 24 (1): 19–26. doi:10.1038/jhh.2009.34. PMID 19474798. S2CID 24409022.
- Parasuraman S, Walker S, Loudon BL, Gollop ND, Wilson AM, Lowery C, Frenneaux MP (September 2016). "Assessment of pulmonary artery pressure by echocardiography-A comprehensive review". International Journal of Cardiology. Heart & Vasculature. 12: 45–51. doi:10.1016/j.ijcha.2016.05.011. PMC 5454185. PMID 28616542.
- Advanced Trauma Life Support (ATLS) Program for Doctors. Chicago, IL: American College of Surgeons. 2008. p. 58. ISBN 978-1-880696-31-6.
- Bertovic DA, Waddell TK, Gatzka CD, Cameron JD, Dart AM, Kingwell BA (June 1999). "Muscular strength training is associated with low arterial compliance and high pulse pressure". Hypertension. Dallas, Texas. 33 (6): 1385–91. doi:10.1161/01.hyp.33.6.1385. PMID 10373221.
- Cushman, William C.; Materson, Barry J.; Williams, David W.; Reda, Domenic J. (1 Oct 2001). "Pulse Pressure Changes With Six Classes of Antihypertensive Agents in a Randomized, Controlled Trial". Hypertension. 38 (4): 953–957. doi:10.1161/hy1001.096212. PMID 11641316.
- Dinallo S, Waseem M (2022). "Cushing reflex". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 31747208.
- Nataf P, Lansac E (September 2006). "Dilation of the thoracic aorta: medical and surgical management". Heart. 92 (9): 1345–1352. doi:10.1136/hrt.2005.074781. PMC 1861150. PMID 16908722.
- Blacher J, Staessen JA, Girerd X, Gasowski J, Thijs L, Liu L, et al. (April 2000). "Pulse pressure not mean pressure determines cardiovascular risk in older hypertensive patients". Archives of Internal Medicine. 160 (8): 1085–1089. doi:10.1001/archinte.160.8.1085. PMID 10789600.
- Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH (April 2017). "Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes". Circulation Research. 120 (9): 1501–1517. doi:10.1161/CIRCRESAHA.117.309732. PMC 5500874. PMID 28450367.
- Khilnani P, Singhi S, Lodha R, Santhanam I, Sachdev A, Chugh K, Jaishree M, Ranjit S, Ramachandran B, Ali U, Udani S, Uttam R, Deopujari S (January 2010). "Pediatric Sepsis Guidelines: Summary for resource-limited countries". Indian J Crit Care Med. 14 (1): 41–52. doi:10.4103/0972-5229.63029. PMC 2888329. PMID 20606908.
- Al-Khalisy H, Nikiforov I, Jhajj M, Kodali N, Cheriyath P (11 December 2015). "A widened pulse pressure: a potential valuable prognostic indicator of mortality in patients with sepsis. J Community Hosp Intern Med Perspect". J Community Hosp Intern Med Perspect. 5 (6): 29426. doi:10.3402/jchimp.v5.29426. PMC 4677588. PMID 26653692.