Fibrate
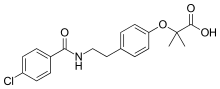
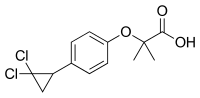
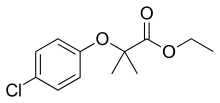
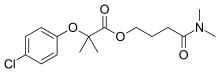
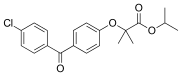
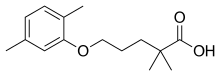
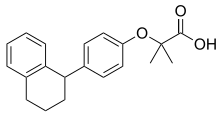
In pharmacology, the fibrates are a class of amphipathic carboxylic acids and esters. They are derivatives of fibric acid (phenoxyisobutyric acid). They are used for a range of metabolic disorders, mainly hypercholesterolemia (high cholesterol), and are therefore hypolipidemic agents.
| Fibrates | |
|---|---|
| Drug class | |
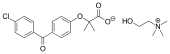
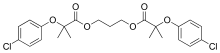
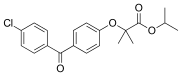 Fenofibrate, one of the most popular fibrates | |
| Class identifiers | |
| Use | hypertriglyceridemia and hypercholesterolaemia |
| ATC code | C10AB |
| Biological target | PPAR |
| Clinical data | |
| WebMD | MedicineNet |
| External links | |
| MeSH | D058607 |
| Legal status | |
| In Wikidata | |
Medical uses
Fibrates improve atherogenic dyslipidemia characterized by high triglyceride and/or low HDL-C levels and elevated concentrations of small dense LDL particles, with or without high LDL-C levels. Fibrates may be compared to statin drugs, which reduce LDL-cholesterol (LDL-C) and have only limited effects on other lipid parameters. Clinical trials have shown that the combination of statins and fibrates results in a significantly greater reduction in LDL-C and triglyceride levels and greater increases in high-density lipoprotein cholesterol (HDL-C) compared with monotherapy with either drug.[1] Fibrates are used in accessory therapy in many forms of hypercholesterolemia, but the combination of some fibrates (e.g., gemfibrozil) with statins is contraindicated due to an increased risk of rhabdomyolysis.[2]
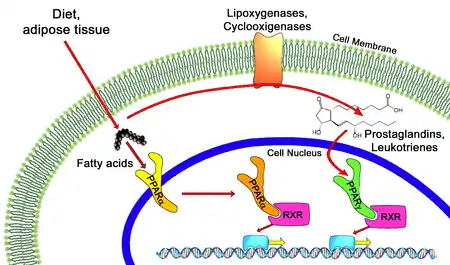
Fibrates stimulate peroxisome proliferator activated receptor (PPAR) alpha, which controls the expression of gene products that mediate the metabolism of triglycerides (TG) and high-density lipoprotein (HDL). As a result, synthesis of fatty acids, TG and VLDL is reduced, whilst that of lipoprotein lipase, which catabolises TG, is enhanced. In addition, production of Apo A1 and ATP binding cassette A1 is up-regulated, leading to increased reverse cholesterol transport via HDL. Consequently, fibrates reduce TG by up to 50% and increase HDL-C by up to 20%, but LDL-C changes are variable. Fewer large-scale trials have been conducted with fibrates than with statins and the results are less conclusive, but reduced rates of cardiovascular disease have been reported with fibrate therapy in the subgroup of patients with low HDL-C levels and elevated TG (e.g. TG > 2.3 mmol/L (200 mg/dL)). Fibrates are usually well tolerated but share a similar side-effect profile to statins. In addition, they may increase the risk of cholelithiasis and prolong the action of anticoagulants. Accumulating evidence suggests that they may also have a protective effect against diabetic microvascular complications.
Clinical trials do support their use as monotherapy agents. Fibrates reduce the number of non-fatal heart attacks, but do not improve all-cause mortality and are therefore indicated only in those not tolerant to statins.[3][4][5]
Although less effective in lowering LDL levels, the ability of fibrates to increase HDL and lower triglyceride levels seems to reduce insulin resistance when the dyslipidemia is associated with other features of the metabolic syndrome (hypertension and diabetes mellitus type 2).[6] They are therefore used in many hyperlipidemias. Due to a rare paradoxical decrease in HDL-C seen in some patients on fenofibrate, as per US FDA label change, it is recommended that the HDL-C levels be checked within the first few months after initiation of fibrate therapy. If a severely depressed HDL-C level is detected, fibrate therapy should be withdrawn, and the HDL-C level monitored until it has returned to baseline.
Side effects
Most fibrates can cause mild stomach upset and myopathy (muscle pain with CPK elevations). Fibrates decrease the synthesis of bile acid by down-regulation of cholesterol 7 alpha-hydroxylase and sterol 27-hydroxylase expression, therefore making it easier for cholesterol to precipitate and increasing the risk for gallstones.
In combination with statin drugs, fibrates cause an increased risk of rhabdomyolysis, idiosyncratic destruction of muscle tissue, leading to kidney failure. The less lipophilic statins are less prone to cause this reaction, and are probably safer to be combined with fibrates than the more lipophilic statins are.
Drug toxicity includes acute kidney injury.[7]
Pharmacology
Although used clinically since at least 1962, the mechanism of action of fibrates remained unelucidated until the 1990s, when it was discovered that fibrates activate peroxisome proliferator-activated receptors (PPARs) , especially PPARα.[8] The PPARs are a class of intracellular receptors that modulate carbohydrate and fat metabolism and adipose tissue differentiation.
Activating PPARs induces the transcription of a number of genes that facilitate lipid metabolism.
Fibrates are pharmacologically related to the thiazolidinediones, a novel class of anti-diabetic drugs that also act on PPARs (more specifically PPARγ)
Fibrates are a substrate of (metabolized by) CYP3A4.[8]
Fibrates have been shown to extend lifespan in the roundworm C. elegans.[9]
Members
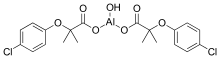
 Choline fenofibrate
Choline fenofibrate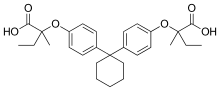

See also
References
- Grundy, Scott M.; Vega, Gloria L.; Yuan, Zhong; Battisti, Wendy P.; Brady, William E.; Palmisano, Joanne (2005). "Effectiveness and tolerability of simvastatin plus fenofibrate for combined hyperlipidemia (The SAFARI trial)". The American Journal of Cardiology. 95 (4): 462–468. doi:10.1016/j.amjcard.2004.10.012. PMID 15695129.
- Steiner G (December 2007). "Atherosclerosis in type 2 diabetes: a role for fibrate therapy?". Diabetes & Vascular Disease Research. 4 (4): 368–74. doi:10.3132/dvdr.2007.067. PMID 18158710. S2CID 31624928.
- Abourbih S, Filion KB, Joseph L, Schiffrin EL, Rinfret S, Poirier P, et al. (October 2009). "Effect of fibrates on lipid profiles and cardiovascular outcomes: a systematic review". The American Journal of Medicine. 122 (10): 962.e1–8. doi:10.1016/j.amjmed.2009.03.030. PMID 19698935.
- Jun M, Foote C, Lv J, et al. (2010). "Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis". Lancet. 375 (9729): 1875–1884. doi:10.1016/S0140-6736(10)60656-3. PMID 20462635. S2CID 15570639.
- Jakob T, Nordmann AJ, Schandelmaier S, Ferreira-González I, Briel M (November 2016). Cochrane Heart Group (ed.). "Fibrates for primary prevention of cardiovascular disease events". The Cochrane Database of Systematic Reviews. 11 (3): CD009753. doi:10.1002/14651858.CD009753.pub2. PMC 6464497. PMID 27849333.
- Wysocki J, Belowski D, Kalina M, Kochanski L, Okopien B, Kalina Z (April 2004). "Effects of micronized fenofibrate on insulin resistance in patients with metabolic syndrome". International Journal of Clinical Pharmacology and Therapeutics. 42 (4): 212–7. doi:10.5414/cpp42212. PMID 15124979.
- Zhao YY, Weir MA, Manno M, Cordy P, Gomes T, Hackam DG, et al. (April 2012). "New fibrate use and acute renal outcomes in elderly adults: a population-based study". Annals of Internal Medicine. 156 (8): 560–9. doi:10.7326/0003-4819-156-8-201204170-00003. PMID 22508733. S2CID 207536477.
- Lee, T.K. "Fibrates in Perspective: Answering an Age-Old Question" (PDF). Perspectives in Cardiology. 20 (6): 34–39.
- Brandstädt, Sven; Schmeisser, Kathrin; Zarse, Kim; Ristow, Michael (2013-04-08). "Lipid-lowering fibrates extend C. elegans lifespan in a NHR-49/PPARalpha-dependent manner". Aging. 5 (4): 270–275. doi:10.18632/aging.100548. PMC 3651519. PMID 23603800.